A virus is a small, infectious agent that is made up of a core of genetic material surrounded by a shell of protein. The genetic material (which is responsible for carrying forward hereditary traits from parent cells to offspring) may be either deoxyribonucleic acid (DNA) or ribonucleic acid (RNA). Viruses are at the borderline between living and nonliving matter. When they infect a host cell, they are able to carry on many life functions, such as metabolism and reproduction. But outside a host cell, they are as inactive as a grain of sand.
Viruses cause disease by infecting a host cell and taking over its biochemical functions. In order to produce new copies of itself, a virus must use the host cell’s reproductive “machinery.” The newly made viruses then leave the host cell, sometimes killing it in the process, and proceed to infect other cells within the organism.
Viruses can infect plants, bacteria, and animals. The tobacco mosaic virus, one of the most studied of all viruses, infects tobacco plants. Animal viruses cause a variety of diseases, including AIDS (acquired immuno deficiency syndrome), hepatitis, chicken pox, smallpox, polio, measles, rabies, the common cold, and some forms of cancer.
Viruses that affect bacteria are called bacteriophages, or simply phages (pronounced FAY-jez). Phages are of special importance due to the susceptibility of the viruse transmission. The disease Polio (poliomyelitis) in time will be transmitted throughout the bloodstream and the highly viral infectious disease is now spreading in the body.
Poliomyelitis (POLIO) is a viral disease. There are three types of poliovirus and many strains of each type. The virus enters through the mouth and multiplies in the throat and gastrointestinal tract, then moves into the bloodstream and is carried to the central nervous system where it replicates and destroys the motor neuron cells. Motor neurons control the muscles for swallowing, circulation, respiration, and the trunk, arms, and legs.
Human nerve cells have a protruding protein structure on their surface whose precise function is unknown. When poliovirus encounters the nerve cells, the protruding receptors attach to the virus particle, and infection begins. Once inside the cell, the virus hijacks the cell’s assembly process, and makes thousands of copies of itself in hours. The virus kills the cell and then spreads to infect other cells.
A virus is a small, infectious agent that is made up of a core of genetic material surrounded by a shell of protein. The genetic material (which is responsible for carrying forward hereditary traits from parent cells to offspring) may be either deoxyribonucleic acid (DNA) or ribonucleic acid (RNA). Viruses are at the borderline between living and nonliving matter. When they infect a host cell, they are able to carry on many life functions, such as metabolism and reproduction. But outside a host cell, they are as inactive as a grain of sand.
How polio is spread:
The virus enters through the mouth and multiplies in the throat and gastrointestinal tract, then moves into the bloodstream and is carried to the central nervous system where it replicates and destroys the motor neuron cells. Motor neurons control the muscles for swallowing, circulation, respiration, and the trunk, arms, and legs.
Human nerve cells have a protruding protein structure on their surface whose precise function is unknown. When poliovirus encounters the nerve cells, the protruding receptors attach to the virus particle, and infection begins. Once inside the cell, the virus hijacks the cell’s assembly process, and makes thousands of copies of itself in hours. The virus kills the cell and then spreads to infect other cells.
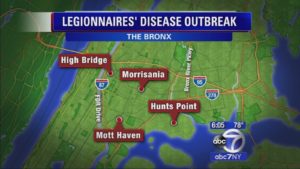
Polio is spread through person-to-person contact. When a child is infected with wild poliovirus, the virus enters the body through the mouth and multiplies in the intestine. It is then shed into the environment through the feces where it can spread rapidly through a community, especially in situations of poor hygiene and sanitation. If a sufficient number of children are fully immunized against polio, the virus is unable to find susceptible children to infect, and dies out. Young children who are not yet toilet-trained are a ready source of transmission, regardless of their environment. Polio can be spread when food or drink is contaminated by feces. There is also evidence that flies can passively transfer polio virus from feces to food. Most people infected with the poliovirus have no signs of illness and are never aware they have been infected. These people with no symptoms carry the virus in their intestines and can “silently” spread the infection to thousands of others before the first case of polio paralysis emerges. For this reason, WHO considers a single confirmed case of polio paralysis to be evidence of an epidemic – particularly in countries where very few cases occur.
The signs and symptoms of Polio:
Most people infected with the poliovirus have no signs of illness and are never aware they have been infected.
These symptomless people carry the virus in their intestines and can “silently” spread the infection to thousands of others before the first case of polio paralysis emerges. For this reason, WHO considers a single confirmed case of polio paralysis to be evidence of an epidemic – particularly in countries where very few cases occur.
Most infected people (90%) have no symptoms or very mild symptoms and usually go unrecognized. In others, initial symptoms include fever, headache, vomiting, stiffness in the neck and pain in the limbs.
Polio is a viral infection!!!
There are three types of poliovirus and many strains of each type.
There are three types of wild poliovirus (WPV):
Type 1, Type 2, and Type 3.
People must protect themselves against all three types of the virus to prevent polio disease.
Polio vaccination is the best protection. There are two vaccines used to protect against polio disease: oral polio vaccine and inactivated poliovirus vaccine.
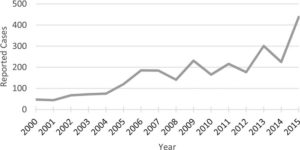
Type 2 wild poliovirus was declared eradicated in September 2015. The last detection was in India, 1999.
Type 3 wild poliovirus was declared eradicated in October 2019. It was last detected in November 2012. Only type 1 wild poliovirus remains.
Presently the CDC states “Type 2 wild poliovirus was declared eradicated in September 2015. The last detection was in India, 1999. Type 3 wild poliovirus was declared eradicated in October 2019. It was last detected in November 2012. Only type 1 wild poliovirus remains.”.
TYPES:
Acute flaccid paralysis (AFP): One in 200 infections leads to irreversible paralysis, usually in the legs. This is caused by the virus entering the blood stream and invading the central nervous system. As it multiplies, the virus destroys the nerve cells that activate muscles. The affected muscles are no longer functional and the limb becomes floppy and lifeless – a condition known AFP = Acute Flaccid Paralysis.
Know all cases of AFP among children under fifteen years old are reported and tested for poliovirus within 48 hours of onset.
All cases of acute flaccid paralysis (AFP) among children under fifteen years of age are reported and tested for poliovirus within 48 hours of onset.
Bulbar polio: More extensive paralysis, involving the trunk and muscles of the thorax and abdomen, can result in quadriplegia. In the most severe cases (bulbar polio), poliovirus attacks the nerve cells of the brain stem, reducing breathing capacity and causing difficulty in swallowing and speaking. Among those paralysed, 5% to 10% die when their breathing muscles become immobilized.
Risk factors for paralysis
No one knows why only a small percentage of infections lead to paralysis. Several key risk factors have been identified as increasing the likelihood of paralysis in a person infected with polio. These include:
- removal of the tonsils (tonsillectomy)
- intramuscular injections, e.g. medications
Treatment and prevention
There is no cure for polio, only treatment to alleviate the symptoms. Heat and physical therapy is used to stimulate the muscles and antispasmodic drugs are given to relax the muscles. While this can improve mobility, it cannot unfortunately reverse permanent polio paralysis.
Polio can be prevented through immunization. Polio vaccine, given multiple times, almost always protects a child for life.