
What is ALS amyotrophic lateral sclerosis?
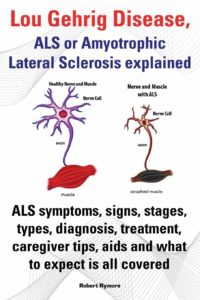
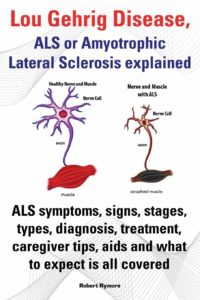
It is a rare neurological disease affecting nerve cells that control voluntary muscle movement. Amyotrophic Lateral Sclerosis or ALS, more commonly known as Lou Gehrig’s disease, is a terminal and progressive motor neuron disease. ALS specifically targets and kills the motor neurons responsible for controlling the vast majority of skeletal muscles in the human body, which eventually leads to respiratory failure and death.
Individuals with ALS experience a degeneration of their motor neurons, which causes the muscles to stop receiving the signals needed to function. After a certain time, the brain completely loses its ability to control voluntary movements, hence, people with ALS are unable to walk, move, or even breathe properly.
ALS belongs to, and is perhaps the most common example of, a group of neurological disorders known as Motor Neuron Diseases. These diseases affect the body by causing the death of millions of neurons found in the motor cortex of the brain as well as the spinal cord. These nerve cells are directly responsible for the regulation and control of skeletal muscle function.
How ALS is diagnosed:
Considering the damage ALS can do, it became essential to spread the message regarding the disease so that people could treat it at an early stage. Though there is no cure for ALS but early detection can help in improving the quality of life of those with the disease.
The signs and symptoms of this diagnosis:
1-Fatigue
A positive diagnosis of ALS is based primarily on a patient’s symptomatology. Unfortunately there is no test that can currently provide a more conclusive assessment.
There are many diseases whose symptoms resemble those observed in patients with ALS. Therefore, diseases such as cervical osteoarthritis, cervical hernias that compress the spinal cord, heavy metal poisoning, and some infectious diseases such as Lyme disease or syphilis, can delay a correct diagnosis of ALS immediately.
As such, when ALS is suspected, it is common practice to rule out other diseases through a variety of tests including but not limited to lumbar punctures, MRIs, and electromyographic studies. In some cases, it might be necessary to perform a biopsy of muscle tissue in order to assuage any remaining doubts.
Often, the earliest symptoms of ALS are ignored or outright dismissed. Therefore, better understand this disease’s signs and symptoms.
2-Loss of strength
Pt’s with ALS eventually lose the ability to control all voluntary movement. During the progression of the disease, which typically lasts for several years, patients will experience a cumulative loss of muscle strength.
In most cases, the first muscles affected by the disease are those of the arms and legs which results in patients experiencing awkwardness when walking or moving about, an increased propensity for stumbling or tripping, and difficulty performing everyday tasks especially fine motor tasks like texting on the phone, typing, and even tying shoe or sneaker laces.
3-Muscle Atrophy
This is when the muscle actually deteriorates and muscle is lost. Leading to muscle dystrophy,in the specific case of ALS, it occurs due to a dramatic reduction in the connection between nerves and muscle fibers caused by the death of motor neurons. It often culminates to paresthesia to partial or total paralysis.
4-Fasciculations
Fasciculations are slight and involuntary muscular contractions that occur underneath the skin, but that do not produce any observable limb movement. Fasciculations are visible to the naked eye and are sometimes described as looking like small worms are moving within the muscle. These contractions occur because of spontaneous nerve discharges that fire within clumps of skeletal muscle fibers. They can occur due to damage present in the lower motor neurons. They could be considered an early warning sign of the possible onset of ALS.
5-Cramps
Muscle cramps are highly common in patients who have ALS, and their incidence increases as the disease progresses. These sustained involuntary contractions of the muscles are typically accompanied by palpable contractures, can last anywhere from 30 to 45 seconds, and tend to be extremely painful. Spasticity could develop and may not allow certain movements as a consequence of cramps; in which antagonistic muscle groups participate.
Other Symptoms include:
- Tripping and falling
- Hand weakness or clumsiness
- Slurred speech or trouble swallowing
- twitching in your arms, shoulders and tongue
- Inappropriate crying, laughing or yawning
- Cognitive and behavioral changes