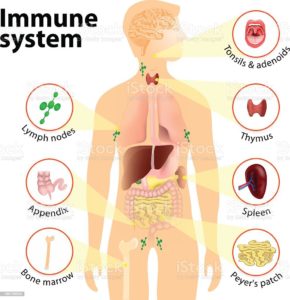
We hear those 2 words “Immune System “a lot; what is the immune system? The main parts of the immune system are:
- white blood cells.
- antibodies.
- complement system.
- lymphatic system.
- spleen.
- bone marrow.
- thymus.
Your immune system is a large network of organs, white blood cells, proteins (antibodies) and chemicals. This system works together to protect you from foreign invaders (bacteria, viruses, parasites, and fungi) that cause infection, illness and disease.
What does the immune system do and how does it work?
Your immune system works hard to keep you healthy. Its job is to keep germs out of your body, destroy them or limit the extent of their harm if they get in.
When your immune system is working properly: When your immune system is working properly, it can tell which cells are yours and which substances are foreign to your body. It activates, mobilizes, attacks and kills foreign invader germs that can cause you harm. Your immune system learns about germs after you’ve been exposed to them too. Your body develops antibodies to protect you from those specific germs. An example of this concept occurs when you get a vaccine. Your immune system builds up antibodies to foreign cells in the vaccine and will quickly remember these foreign cells and destroy them if you are exposed to them in the future. Sometimes doctors can prescribe antibiotics to help your immune system if you get sick. But antibiotics only kill certain bacteria. They don’t kill viruses.
When your immune system is not working properly: When your immune system can’t mount a winning attack against an invader, a problem, such as an infection, develops. Also, sometimes your immune system mounts an attack when there is no invader or doesn’t stop an attack after the invader has been killed. These activities result in such problems as autoimmune diseases and allergic reactions.
Your immune system is made of up a complex collection of cells and organs. They all work together to protect you from germs and help you get better when you’re sick. The main parts of the immune system are:
- White blood cells: Serving as an army against harmful bacteria and viruses, white blood cells search for, attack and destroy germs to keep you healthy. White blood cells are a key part of your immune system. There are many white blood cell types in your immune system. Each cell type either circulates in your bloodstream and throughout your body or resides in a particular tissue, waiting to be called into action. Each cell type has a specific mission in your body’s defense system. Each has a different way of recognizing a problem, communicating with other cells on the defense team and performing their function.
- Lymph nodes: These small glands filter and destroy germs so they can’t spread to other parts of your body and make you sick. They also are part of your body’s lymphatic system. Lymph nodes contain immune cells that analyze the foreign invaders brought into your body. They then activate, replicate and send the specific lymphocytes (white blood cells) to fight off that particular invader. You have hundreds of lymph nodes all over your body, including in your neck, armpits, and groin. Swollen, tender lymph nodes are a clue that your body is fighting an infection.
- Spleen: Your spleen stores white blood cells that defend your body from foreign invaders. It also filters your blood, destroying old and damaged red blood cells.
- Tonsils and adenoids: Because they are located in your throat and nasal passage, tonsils and adenoids can trap foreign invaders (for example, bacteria or viruses) as soon as they enter your body. They have immune cells that produce antibodies to protect you from foreign invaders that cause throat and lung infections.
- Thymus: This small organ in your upper chest beneath your breast bone helps mature a certain type of white blood cell. The specific task of this cell is to learn to recognize and remember an invader so that an attack can be quickly mounted the next time this invader is encountered.
- Bone marrow: Stem cells in the spongy center of your bones develop into red blood cells, plasma cells and a variety of white blood cells and other types of immune cells. Your bone marrow makes billions of new blood cells every day and releases them into your bloodstream.
- Skin, mucous membranes and other first-line defenses: Your skin is the first line of defense in preventing and destroying germs before they enter your body. Skin produces oils and secretes other protective immune system cells. Mucous membranes line the respiratory, digestive, urinary and reproductive tracts. These membranes secrete mucus, which lubricates and moistens surfaces. Germs stick to mucus in the respiratory tract and then are moved out of the airways by hair-like structures called cilia. Tiny hairs in your nose catch germs. Enzymes found in sweat, tears, saliva and mucus membranes as well as secretions in the vagina all defend and destroy germs.
- Stomach and bowel: Stomach acid kills many bacteria soon after they enter your body. You also have beneficial (good) bacteria in your intestines that kill harmful bacteria.