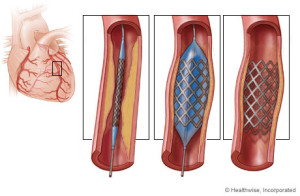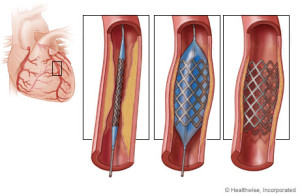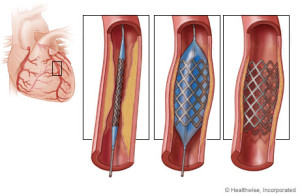
A stent is a wire mesh tube that is used to help hold open an artery. To simple understanding this concept think of a plumber or a mechanic. With a plumber sometimes they have to replace a certain area of a pipe that connects the water or like a mechanic replacing a certain area of piping (like the muffler piping connected infront of the muffler than can either can be replaced or just welded with piece of piping welded just to save money. Well a stent opens the artery that was clogged and its put in that place to reinforce that area of the artery to remain open to allow blood to get to that heart from that coronary artery and it will stay there life to keep the artery permanently patent to prevent the blockage from happening again with the synthetic mesh piece.
Description
Stents are used to hold open diseased coronary arteries (these arteries supply blood to the heart), as well as diseased arteries of the peripheral vascular system (PVS). Peripheral means away from the heart the PVS is the arteries that supply blood to the rest of the body (again away from the heart all the way down to the hands and feet).
There are variety of stents currently available.
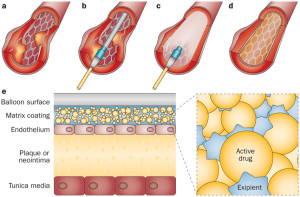
For a surgeon to find out if you even need one, first usually a angiogram is performed and this is a catheter simply from the femerol artery or from your arm to the coronary arteries. If the MD sees you show a blockage 80% or more an angioplasty is performed which is a balloon at the end of this catheter that blows up and decompresses to give the effect like punching gloves. The balloon inflates and deflates over and over again till the blockage breaks open free and then a stent is put in that area to help keep it open permanently (patent).
Some stents have been compressed onto the outside of an angioplasty balloon catheter and delivered by inflating the balloon in the desired location. Other stents are “self- expanding” spring-loaded devices, which expand automatically upon deployment.
Stents remain in arteries permanently. The tissue lining the arteries actually grows over the metal mesh to cover the inner lumen of the stent.
Stent procedures have become very common like tonsillectomies were in childhood. Stents are sometimes used as an alternative to coronary artery bypass surgery, if the patient is a candidate. Stents are often used in combination with balloon angioplasty. One leads to the other depending on what the angioplasty displays for the surgeon on the T.V. in when they are doing the procedure and if the come up to a blockage high enough to perform the angioplasty followed with a stent it will be done.
Stents are used in cases of “restenosis”, which refers to the re-closing of arteries after balloon angioplasty. In carefully selected patients, the use of stents can dramatically reduce restenosis following balloon angioplasty or other catheter-based procedures. Stents are used frequently to hold open the arteries that have been damaged, torn, or dissected by balloon angioplasty or other catheter-based procedures. Like plumber or mechanic, get it.
Stents allow angioplasty to be done in patients with severe and long-segment obstruction of coronary arteries. As soon as the I initial part of the block is widened, a stent is place, which holds it open allowing further opening to proceed. Stents have also allowed angioplasty to be performed in patients with blocks of multiple vessels, and in multiple blocks in a single artery.
Angioplasty and stent placement are common procedures to open arteries in the heart that are clogged. These procedures are formally known as coronary angioplasty or percutaneous coronary intervention.
Angioplasty involves the use of a tiny balloon to widen the artery. A stent is a tiny wire-mesh tube that your doctor inserts into the artery. The stent stays in place to prevent the artery from closing. A cardiologist typically performs both procedures at the same time.
While angioplasty with stent placement addresses an individual blockage, it doesn’t fix the underlying cause of the blockage. To prevent further blockages and reduce your risk of other medical conditions, you may have to make certain lifestyle changes to prevent it happening again. The procedure of the angioplasty to insert a stent if needed resolves the immediate acute problem that the underlining disease the pt had causing the blockage. This could be due to high cholesterol, diabetes, CAD, and atheroscerosis.