This holiday can be traced all the way back to 2002. This is when the day was established by the American Heart Association and National Heart, Lung and Blood Institute. Every year since its inception, this campaign has continued to reach a higher audience. This has resulted in greater awareness about heart disease and how it affects women.
National Wear Red Day isn’t an official holiday, so government buildings, post offices, and businesses remain open on this day. On this day, many people wear red to promote heart-health awareness among women. Some people also use this day to raise money for various heart-related charities such as the American Heart Association. On social media, many people will use the hashtag #GoRedWearRed to help bring attention to the day.
People wear red as a way to bring attention to the problem of heart disease in women. Many women wear red dresses (or other clothing too in red), the identifying symbol for the day. Health organizations hold seminars and public outreach events to educate people about prevention and screening of heart disease.
It’s also a good day for women to get their numbers checked. Having your blood pressure, cholesterol and triglyceride levels, blood sugar and BMI checked is a good way to find out if you’re at risk for developing heart disease.
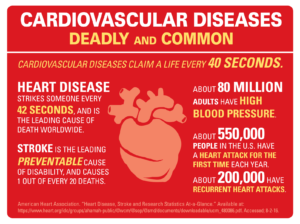
Some Heart Disease Facts that could help many lives and possibly open some eyes to see the doctor at least yearly:
- Heart disease kills one woman every 80 seconds
- Every year, 30% of the deaths among women in the U.S are caused by heart attacks and strokes.
- 64% of women who die suddenly from heart disease will have no prior symptoms
- High cholesterol, high blood pressure, diabetes, obesity and smoking all contribute to heart disease
- Physical inactivity also is a contributing factor to heart disease
All women face the threat of heart disease. Knowing the symptoms and risks unique to women, as well as eating a heart-healthy diet and exercising, can help protect you.
Heart disease is often thought to be more of a problem for men. However, it’s the most common cause of death for both women and men in the United States. Because some heart disease symptoms in women can differ from those in men, women often don’t know what to look for.
Fortunately, by learning their unique heart disease symptoms, women can begin to reduce their risks.
What is actually Heart Disease mean?
Conditions of the heart including structural and functional abnormalities which is pretty much all the heart illnesses and all the diagnosis(s). This is HTN, heart attack, heart failure, Coronary Heart Disease, Atrial fibrillation, etc…
Biggest factor in preventing heart disease is staying healthy, great eating habits, letting your primary care doctor know family cardiac history especially in the nuclear family which will guide the M.D. in knowing what to look for in particular from assessments to tests yearly.