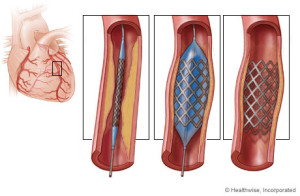
Stents are used in cases of “restenosis”, which refers to the re-closing of arteries after balloon angioplasty. In carefully selected patients, the use of stents can dramatically reduce restenosis following balloon angioplasty or other catheter-based procedures. Stents are used frequently to hold open the arteries that have been damaged, torn, or dissected by balloon angioplasty or other catheter-based procedures. Like plumber or mechanic, get it.
Stents allow angioplasty to be done in patients with severe and long-segment obstruction of coronary arteries. As soon as the I initial part of the block is widened, a stent is place, which holds it open allowing further opening to proceed. Stents have also allowed angioplasty to be performed in patients with blocks of multiple vessels, and in multiple blocks in a single artery.
Risks of getting cardiac stents:
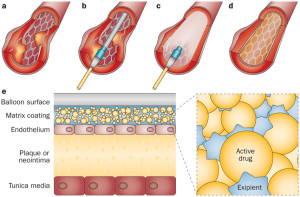
Risks include the standard risks of an interventional, catheter-based procedure, which should be specifically discussed with your doctor. Lesions treated with stents can “restenosis” (re- narrow with in weeks to months after the procedure) similar to restenosis associated with angioplasty. This is why patients after having a stent put in they are on a medication for example like Plavix for life to prevent this occurrence from happening. It is a anti platelet medication, meaning it doesn’t allow clotting to happen in the stent so blockage doesn’t reoccur through clotting.
Many new technologies are being tested to reduce the problem of restenosis, meaning close up. These technologies include coating and coverings for the stent, new materials, and radiation. These new technologies are primarily experimental at this point and will reach soon to the market if not already. Technology allows the medical field to continuously expand and this will be replaced at one point but isn’t yet. Just give it time. At one point we had no CABG (coronary artery bypass) but now the stent in certain cases is replaced by angiograms to further expanding to angioplasties and stents furthering allowing the surgery to take place 1x hopefully if the patient is compliant in diet, exercise, and following the doctors orders with meds, activity and follow up visits (which are so vital). A lot is up to the patient in caring for themselves to prevent having this take place again.
St John’s Hopkins Medicine states that the risks of getting a stent are the following:
Possible risks linked to angioplasty, stenting, atherectomy, and related procedures include:
- Bleeding at the site where the catheter is put into the body (usually the groin, wrist, or arm)
- Blood clot or damage to the blood vessel from the catheter
- Blood clot within the treated blood vessel
- Infection at the catheter insertion site
- Abnormal heart rhythms
- Heart attack
- Stroke
- Chest pain or discomfort
- Rupture of the coronary artery or complete closing of the coronary artery, needing open-heart surgery
- Allergic reaction to the contrast dye used
- Kidney damage from the contrast dye
Follow up Instructions
Your doctor will recommend blood thinning medications following your stent procedure. These agents are usually given for one month post procedure along with aspirin and then continued indefinitely. Your doctor may also prescribe antibiotics for a period of time after the stent procedure, to be taken anytime you have a medical or dental procedure. Preventing infection.
MRI tests should not be done for at least eight weeks without your doctor’s approval. Metal detectors do not present a problem. Stents appear to be safe in the long-term; there are no long-term complications associated with a permanent stent.