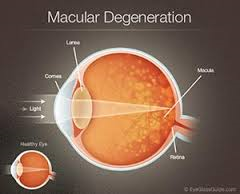
Age-related macular degeneration (AMD) is a deterioration or breakdown of the eye’s macula. The macula is a small area in the retina — the light-sensitive tissue lining the back of the eye. The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly.
The macula makes up only a small part of the retina, yet it is much more sensitive to detail than the rest of the retina (called the peripheral retina). The macula is what allows you to thread a needle, read small print, and read street signs. The peripheral retina gives you side (or peripheral) vision. If someone is standing off to one side of your vision, your peripheral retina helps you know that person is there by allowing you to see their general shape.
Many older people develop macular degeneration as part of the body’s natural aging process. There are different kinds of macular problems, but the most common is age-related macular degeneration.
Signs and symptoms of Macular Degenerative Disease:
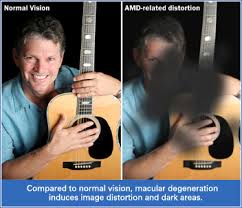
With macular degeneration, you may have symptoms such as blurriness, dark areas or distortion in your central vision, and perhaps permanent loss of your central vision. It usually does not affect your side, or peripheral vision. For example, with advanced macular degeneration, you could see the outline of a clock, yet may not be able to see the hands of the clock to tell what time it is.
- Blurry distance and/or reading vision
- Need for increasingly bright light to see up close
- Colors appear less vivid or bright
- Hazy vision
- Difficulty seeing when going from bright light to low light (such as entering a dimly lit room from the bright outdoors)
- Trouble or inability to recognize people’s faces
- Blank or blurry spot in your central vision. * The risks of Macular Degeneration: For Developing Age-Related Macular Degeneration
The risk factors we can control=Modifiable Rish Factors:
- Smoking: Current smokers have a two-to-three times higher risk for developing age-related macular degeneration than people have who never smoked.
- Artificial fats: Usually labeled “partially-hydrogenated vegetable oils,” these artificial fats are pervasive in foods and particularly in low-fat bakery goods. Low-fat foods are good options if they’ve achieved their low-fat status through a process that physically removes the fat, as in skim milk or low-fat cottage cheese. Low-fat bakery goods are different, however. If you remove all or half the fat from a cake recipe, it won’t turn into a cake; thus, when cakes and bakery goods are labeled low-fat or no-fat, it means they contain artificial fats, or laboratory-produced chemicals. These chemicals are not food and our bodies can’t metabolize them.
- Sunlight: It is the blue wavelengths from the sun that damage the macula, not the ultraviolet (UV) rays.
- A diet high in processed, packaged foods and low in fresh vegetables: Vegetable oils are added in the packaging process. These oils are rich in omega-6 fatty acids, which promote inflammation.
- Uncontrolled hypertension and high cholesterol: Research by the National Eye Institute indicates that persons with hypertension are 1.5 times more likely to develop wet macular degeneration than persons without hypertension.
- Obesity: Being overweight doubles the risk of developing advanced macular degeneration.
The four risk factors we can’t control=Unmodifiable Risk Factors:
- Advanced age: Although AMD may occur earlier, studies indicate that people over age 60 are at greater risk than those in younger age groups. For instance, a large study found that people in middle age have about a 2% risk of getting AMD, but this risk increased to nearly 30 percent in those over age 75.
- Race: Whites are much more likely to lose vision from age-related macular degeneration than are Blacks or African-Americans.
- A gene variant that regulates inflammation: While not all types of macular degeneration are hereditary, certain genes have been strongly associated with a person’s risk of age-related macular degeneration, and genetic predisposition may account for half the cases of age-related macular degeneration in this country.
- Family history: Studies indicate that your chances of developing age-related macular degeneration are three to four times higher if you have a parent, child, or sibling with macular degeneration.
Treatment of Macular Degeneration:
People who develop significant age-related macular degeneration (AMD) typically compensate with large-print publications and magnifying lenses for everyday activities. In addition, evidence suggests that certain vitamins and antioxidants — vitamins C and E, beta-carotene, and zinc — may help reduce or delay the risk of severe vision loss. Ask your eye doctor about using nutritional supplements.
1. Treatment for Dry Macular Degeneration
Dry macular degeneration, the most common form of AMD, cannot be cured at this time, but patients with the condition should continue to remain under an ophthalmologist’s care to monitor both eyes. If the one eye is healthy, screening should still continue.
2. Treatment for Wet Macular Degeneration
A variety of treatments are available for wet AMD. Successful treatment may not restore normal vision, but it will improve sight and prevent central vision loss from worsening. While laser procedures can destroy the abnormal blood vessels, they also damage neighboring retinal tissue.
Medications, such as Eylea, Lucentis, and Macugen, have become the preferred treatment for acute wet macular degeneration, helping to prevent the growth of leaky blood vessels in your eye. Lucentis is given once every month, although some patients may need treatment only once every three months. Macugen is given every six weeks. Eylea is given once every two months after three once-monthly injections.
Laser photocoagulation destroys leaking blood vessels that have grown under the macula and halts the leakage. Laser therapy is helpful for about 10%-20% of people with wet macular degeneration. Some vision loss may occur, because this treatment creates scar tissue that is perceived as blind spots; however, even more vision would be lost if nothing is done at all. Up to half of patients who elect laser therapy may need repeat treatments.
Photodynamic therapy (PDT) uses a different, non-heat-generating laser to treat abnormal blood vessels. Visudyne is injected into the patient’s arm and flows through the vessels in the eye. Upon exposure to the laser, a chemical reaction occurs that seals off the leaky vessels. Since the dye is light sensitive, you must stay out of the sun or bright light for several days until the dye has passed from your system. Laser photocoagulation must be done before the abnormal blood vessels cause irreversible damage to the retina. More blood vessels could grow later on, so people who undergo this treatment also need to continue with regular follow-up appointments.
Vitamins. A large study performed by the National Eye Institute of the National Institutes of Health, called AREDS (Age-Related Eye Disease Study), showed that for certain individuals, vitamins C, E, beta-carotene, zinc and copper can decrease the risk of vision loss in patients with intermediate to advanced dry macular degeneration. In addition, there was a correlation between the hormone DHEA and the degree of macular degeneration. DHEA can be purchased over-the-counter.