LOOKING AT ACTUAL STUDIES SUPPORTING OBESITY&CANCER LINK
Take for example through the American Cancer Society they stated in an article 2006 that a substantial evidence from clinical trials has established that obesity significantly increases the risk for heart disease and diabetes. More recently, suspicions that obesity is linked to prostate cancer have been supported by a number of investigations, but the relationship has remained unclear. Now through a pair of new studies provides scientists with some important insights that may have an impact on how physicians manage their patients with prostate cancer.
The pair of studies show 2 significant studies relating how obesity links with prostate cancer, which were:
The implication is that prostate cancer patients who are obese should probably be followed more closely than patients with similar cancer characteristics who are not obese. That could include regular digital rectal exams, more frequent prostate-specific antigen (PSA) testing, and perhaps setting a lower PSA cutoff point as an indication of recurrence, Kane explained.
The greater risk associated with obesity may be related to technical issues, Kane said. For example, it’s more difficult for surgeons to perform a radical prostatectomy in obese patients. However, surgical challenges offer only a partial explanation. In studies where surgeons verified that they had removed all cancer cells during radical prostatectomy, obese patients were still more likely to experience a recurrence of the disease.
The second study, a multi-center trial coordinated at the Duke University School of Medicine in Durham, NC, found that obese men under the age of 63 tend to have larger prostates, which makes finding tumors more difficult. As a result, there’s a real danger of delayed diagnosis, which decreases the chances of a cure and puts patients at greater risk for dying of the disease. The findings appear in the Journal of Urology.
“It’s harder to find cancer in larger prostate glands,” explained Stephen J. Freedland, MD, assistant professor of urology and member of the Duke Prostate Center at the Duke University School of Medicine. “Consequently, our data suggest that we may be underdiagnosing cancers in younger obese men. That also means that the tumors we do pick up are likely to be at a more advanced stage and perhaps more aggressive, and therefore more difficult to treat.”
Let’s look at this at a broader aspect, not just pertaining to prostate cancer. This would be, “It’s not just patients with prostate cancer that studies like this should be directed toward,” Dr. Kane said. “Patients who are clearly at risk for developing the disease should also take notice of our findings. The central message is yet again that obesity has been identified as an important risk factor for a potentially deadly disease. For all of us, controlling our weight through diet and exercise is important, and we shouldn’t have blinders on and just think of prostate cancer. The number one risk of death for American men is heart disease, so anything we can do to reduce that risk that also reduces the risk for prostate cancer is useful.” Including it reduces risk for other cancers as well that are impacted by disease, it makes sense.
Obesity links to an increased risk of ovarian cancer. Let’s look at this no: Atlanta 2009/01/05 -A new epidemiological study has found that among women who have never used menopausal hormone therapy, obese women are at an increased risk of developing ovarian cancer compared with women of normal weight. Published in the February 15, 2009 issue of CANCER, a peer-reviewed journal of the American Cancer Society, the research indicates that obesity may contribute to the development of ovarian cancer through a hormonal mechanism. Ovarian cancer is the most fatal of gynecologic malignancies, and has a 5-year survival rate of only 37 percent.
To investigate this issue, Dr. Michael F. Leitzmann of the National Cancer Institute and colleagues studied 94,525 U.S. women aged 50 to 71 years over a period of seven years. The researchers documented 303 ovarian cancer cases during this time and noted that among women who had never taken hormones after menopause, obesity was associated with an almost 80 percent higher risk of ovarian cancer. In contrast, no link between body weight and ovarian cancer was evident for women who had ever used menopausal hormone therapy.
According to Dr. Leitzmann, these findings support the hypothesis that obesity may enhance ovarian cancer risk in part through its hormonal effects. Excess body mass in postmenopausal women leads to an increased production of estrogen, which in turn may stimulate the growth of ovarian cells and play a role in the development of ovarian cancer.
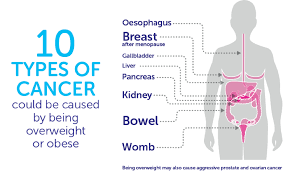
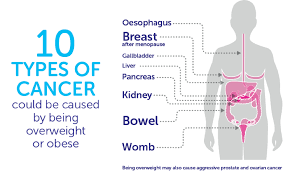
In another study done 2003, American Cancer Society researchers analyzed data based on 900,000 American adults with obesity and cancer that they monitored for a total of 16 years. This is what they found in their landmark study: 1)The researchers found that the most obese women had a 62% increase in their risk of dying from cancer than women of normal weight; for obese men, the increase was 52%. The wide range of tumor types included colorectal, liver, gallbladder, pancreas, esophageal, kidney, prostate, breast, uterine, endometrial, and ovarian cancers. The researchers conclusion was that above-normal weight was associated with almost 20% of all cancer deaths in the United States. “There’s an incredibly powerful link between obesity and cancer,” says oncologist Joyce Slingerland of the University of Miami, Florida. “Everyone’s heard of obesity’s effect on heart disease and diabetes, and we’re now beginning to understand that the cancer risk is just as great,” she says.
Although researchers and epidemiologists had long suspected that diet and cancer were linked, efforts to explain why being fat makes cancer more deadly have only begun to deliver results in the past decade.
So it is up to the people in society of that country they live in to take on responsible actions to make their country a better for all, not just one. I say that is becoming as healthy as possible that an individual can reach and without America has the answers in knowing how to make this happen 100% in our country.
A new study from American Cancer Society researchers finds it’s not just how much physical activity you get, but how much time you spend sitting that can affect your risk of death.
My final study supporting how obesity links with cancer:
Just think if this was you or someone you know in the world and this happens to you or them; GOD FORBID, but you can help yourself through prevention with losing the weight or just staying slim and tone if you already are. This will just decrease your risk of getting the cancer.
The JCCC study, led by Dr. Guido Eibl, JCCC member and professor-in-residence in the department of surgery at David Geffen School of Medicine, revealed that mice made obese with high-calorie, high-fat diets developed abnormally high numbers of these lesions.
This is the first study to show a direct causal link in an animal model between obesity and risk of this deadly pancreatic cancer.
The JCCC study, led by Dr. Guido Eibl, JCCC member and professor-in-residence in the department of surgery at David Geffen School of Medicine, revealed that mice made obese with high-calorie, high-fat diets developed abnormally high numbers of these lesions. This is the first study to show a direct causal link in an animal model between obesity and risk of this deadly pancreatic cancer.
The mice eating the normal diet gained an average of approximately 7.2 g over 14 months. Mice on the high-fat, high-calorie diet more than doubled this with an average weight gain of 15.9 g.
Pathological tests showed that mice fed the normal diet had mostly normal pancreases with very few scattered PanIN lesions=intraepithelial neoplasias=precursors to pancreatic lesions. They are used as markers but can only be seen microscopically so a biopsy is needed. The mice fed high fat & cholesterol in their diet had significantly more PanIN lesions with less overall healthy pancreases.
The study showed that the mice fed a diet high in fats and calories gained significantly more weight, had abnormalities of their metabolism and increased insulin levels, and had marked pancreatic tissue inflammation with the development of PanIN lesions.
These observations suggest that such a diet like this which leads to weight gain, metabolism disturbances, pancreas inflammation and pancreas lesions that are precursors to cancer.
Obviously research is showing obesity has a link with cancer. We now know this information let’s make a move America and people elsewhere to become a healthier nation including world. For diversity is the US and other countries filled with all cultures, races and genders need to learn this knowledge to help make their country whether they were either born there and stayed or those born elsewhere moving to a new country, like America and we the people making up the country need to be responsible not just for yourselves but for your children and future generations in spreading good habits, good dieting, and good exercise to prevent high disease in the country for yourself and your children and the future generations by being a good role model in thinking=live healthy not unhealthy. In time this would play an impact on your countries economy and health care system in how its run. So come with me, like many others if you need to know the simple steps in how to go about losing weight safely but easy with learning better healthy habits and practicing some form of exercise which will benefit you in having a healthier body than join me at my website healthyusa.tsfl.com and become a member with getting guidance through Dr. Anderson on his healthy habits through his book and me as your health coach. Take a peek you might just like what you see. You make all the choices in what you want and going to the site costs nothing. There will come a point you get your routine down and don’t need our help with staying healthy for life with decreasing your chance of so many diseases, not just cancer, from occurring. Help me with so many others in tring to make a difference in America by becoming healthier. Slowly but surely I am and I know you can to at your pace.
References:
1 –American Institute for Cancer Research, Schernhammer ES et al. Circulating levels of insulin-like growth factors, their binding proteins, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2005 Mar;14(3):699-704 ES et al. their binding proteins, and breast cancer risk— Cancer Epidemiol Biomarkers Prev. 2006 Mar;14(3):699-704/ AICR ScienceNow /Volume 16/Spring 2006
2 – Studies Help Clarify Link Between Obesity and Prostate Cancer Article date: March 2, 2006 Impact of Obesity on Prostate Cancer Recurrence After Radical Prostatectomy: Data from CaPSURE.” Published in the Nov., 2005 Urology (Vol. 66, No. 5: 1060-1065). First author: William W. Bassett, University of California, San Francisco.
“Obesity, Serum Prostate Specific Antigen and Prostate Size: Implications for Prostate Cancer Detection.” Published in the Feb. 2006 Journal of Urology (Vol. 175, No. 2: 500-504). First author: Stephen J. Freedland, MD, Duke University School of Medicine.
3 – Director, Medical & Scientific Communications American Cancer Society david.sampson@cancer.org Article: “Body mass index and risk of ovarian cancer.” Michael F. Leitzmann, Corinna Koebnick, Kim N. Danforth.