Arlen Specter ((February 12, 1930 – October 14, 2012) was a United States Senator from Pennsylvania
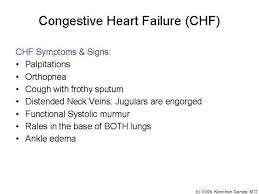
Part 2-CHF (heart failure) Signs&Symptoms/Diagnosis and Prevention
A number of symptoms are associated with heart failure, but none is specific for the condition. Perhaps the best known symptom is short of breath (called dyspnea). In heart failure, this may result from excess fluid in the lungs. The breathing difficulties may occur at rest or during exercise. In some cases, congestion may be severe enough to interrupt or prevent you from sleeping.
-Fatigue or easy tiring is another common symptom. As the heart’s pumping capacity decreases, muscles and other tissues receive less oxygen and nutrition, which are carried in the blood. Without proper fuel (oxygen from the blood) provided by our engine (the heart), the body cannot perform as much work as it use to do (just like going from in shape to out of shape in time). The ending line is this will result into fatigue.
-Fluid accumulation will cause swelling in the feet, ankles, legs, and occasionally the abdomen (if the fluid building up in the body gets severe), what we medically call edema. Through gravity the blood goes backwards and our body allows water to transfer in the skin to allow the fluid to go somewhere other than the bloodstream to decrease fluid overload to the heart by compensating. It body compensates since the blood is going backwards from the heart causing fluid back up. Excess fluid retained by the body will result into weight gain, which sometimes occurs fairly quickly (if you have CHF already you should always call your M.D. if you weight gain is 3lbs or more in a week, odds are high this is due to fluid building up).
-Persistent coughing is another common sign, especially coughing that regularly produces mucus or pink, blood-tinged sputum. Some people develop raspy breathing or wheezing.
Heart failure usually goes through a slow development process, the symptoms may not appear until the condition has progressed over the years. This happens because the heart first compensates by making adjustments with the heart that delay or slow down but do not prevent, the eventual loss in pumping capacity. In time failure happens, just like a car in when it gets older over several years is starts showing one problem after another and is exchanged for a newer car; same principle with the heart in that you show signs and symptoms as your heart starts to slow down to failure and its either treat the problem or get a transplant of the organ (which is unlikely to happen). The heart first hides the underlying process but compensates by doing this to your heart:
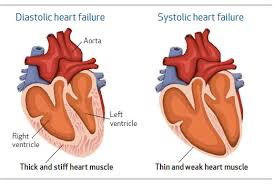
1- Enlargement to the muscle of the heart (causing “dilatation”) which allows more blood into the heart.
2- Thickening of muscle fibers (causing “hypertrophy”) to strengthen the heart muscle, which allows the heart to contract more forcefully and pump more blood.
3- More frequent contraction, which increases circulation.
By making these adjustments, or compensating, the heart can temporarily make up for losses in pumping ability, sometimes for years. However, compensation of the organ can only last so long, not forever (like anything in life the living thing or an object will go through a ending life process to termination). Eventually the heart cannot offset the lost ability to pump blood, and the signs of heart failure appear.
DIAGNOSIS
In many cases, physicians diagnose heart failure during a simple physical examination. Readily identifiable signs are shortness of breath, fatigue, and swollen ankles and feet. The physician also will check for the presence of risk factors, such as hypertension, obesity and a history of heart problems.
Using a stethoscope, the physician can listen to a patient breathe and identify the sounds of lung congestion. The stethoscope also picks up the abnormal heart sounds indicative of heart failure.
If one or not both symptoms or the patient’s history point to a clear cut diagnosis, the physician may recommend any of a variety of laboratory tests, including, initially, an electrocardiogram (EKG), which uses recording devices placed on the chest to evaluate the electrical activity of a patient’s heartbeat which will be affected by CHF.
Echocardiography is another means of evaluating heart function from outside the body. This works through sound waves that bounce off the heart are recorded and translated into images. The pictures can reveal abnormal heart sizes, shape, and movement. Echocardiography also can be used to calculate a patient’s ejection fraction which is a measurement of the amount of blood pumped when the heart contracts.
Another possible test is the chest x-ray, which also determines the heart’s size and shape, as well as the presence of congestion in the lungs.
Tests help rule out other possible causes of symptoms. The symptoms of heart failure can result when the heart is made to work too hard, instead of from damaged muscle (like in a heart attack). Conditions that overload the heart occur rarely and include severe anemia and thyrotoxicosis (a disease resulting from an overactive thyroid gland).
Prevention of CHF:
-If not diagnosed yet your already possibly ahead. Without this diagnosis you can get started on making yourself further away from being diagnosed with this disease. How to reach this goal is through living a routine life through healthy habits practiced, healthy dieting over all, and balancing rest with exercise during the week 30-40 minutes a day or 1 hour to 1.5 hours 3 times a week and not being obese. They all would benefit the heart in not stressing it out making the heart’s function harder in doing its function. When the heart stresses out it is at risk for lacking oxygen putting it at potential for angina (heart pain) to a heart attack with over time leading toward failure of the heart. Need to learn more about what is and how to get your weight in therapeutic body mass index range through dieting of all 4 food groups, balancing exercise/rest, and knowing how the body works with all ingredients in foods including portion sizes (fats, calories, starches, carbohydrates, proteins with vitamins and minerals) to understanding how all this information takes effect in how your metabolism operates in being beneficial or against you? Than get into a workout place or just go to channels on TV/cable that offer classes for free, read up on good foods vs. bad foods as simple as on the internet or even again TV/cable channels and balance rest with exercise; it is just taking action and doing what you need to stay healthy for the heart. Remember staying healthy for the heart is being healthy for so many other areas of the body (the heart is the engine to the body).;)
QUOTE FOR MONDAY:
“Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs.”
NIH National Heart Lung and Blood Institute
QUOTE FOR THE WEEKEND:
“Ablation therapy is a type of minimally invasive procedure doctors use to destroy abnormal tissue that occurs with many conditions. For example, your doctor may use an ablation procedure to treat or to destroy (ablate) a small amount of heart tissue that’s causing abnormally rapid heart rhythms.”
MAYO CLINIC
QUOTE FOR FRIDAY:
“The general population has about a 1% risk of developing epilepsy. Meanwhile, children of mothers with epilepsy have a 3 to 9% risk of inheriting this disease, while children of fathers have a 1.5 to 3% risk of inheritence.” Based on genes research
Dr. Robert S. Fischer Ph D. Stanford Epilepsy Center
QUOTE FOR THURSDAY:
“Women have more colds than men, and this is probably due to increased interaction with children, children get around seven to ten colds a year, compared with two to three for adults. So people who spend a lot of time with children, such as childminders, nursery teachers or school teachers, are more likely to pick up the viruses.”
Professor Eccles of the Common Cold Centre in Cardiff
QUOTE FOR WEDNESDAY:
Part III Cushing’s Syndrome – Diagnosing it and Treatment for it.
How is Cushing’s syndrome diagnosed and treated?
Diagnosis is established on a survey of the patient’s medical history including somatic examination and laboratory tests.
Frequently x-ray exams of the adrenal or pituitary glands are beneficial for locating tumors. These tests assist to find out if excess levels of cortisol are exhibited and why.
Radiologic imaging: direct visualization of the endocrine glands. Imaging tests reveal the size and shape of the pituitary and adrenal glands and help determine if a tumor is present. The most common imaging tests are the computerized tomography (CT) scan and magnetic resonance imaging (MRI). A CT scan produces a series of x-ray pictures giving a cross-sectional image of a body part. MRI also produces images of internal organs but without exposing patients to ionizing radiation.
Imaging procedures are used to find a tumor after a diagnosis has been made. Imaging is not used to make the diagnosis of Cushing’s syndrome because benign tumors are commonly found in the pituitary and adrenal glands. These tumors, sometimes called incidentalomas, do not produce hormones in quantities that are harmful. They are not removed unless blood tests show they are a cause of symptoms or they are unusually large. Conversely, pituitary tumors may not be detectable by imaging in almost half of people who ultimately need pituitary surgery for Cushing’s syndrome.
24-hour urinary free cortisol level. In this test, a person’s urine is collected several times over a 24-hour period and tested for cortisol. Levels higher than 50 to 100 micrograms a day for an adult suggest Cushing’s syndrome. Low-dose dexamethasone suppression test (LDDST). In the LDDST, a person is given a low dose of dexamethasone, a synthetic glucocorticoid, by mouth every 6 hours for 2 days. Urine is collected before dexamethasone is administered and several times on each day of the test. A modified LDDST uses a onetime overnight dose.
The normal upper limit varies in different laboratories, depending on which measurement technique is used.
Midnight plasma cortisol and late-night salivary cortisol measurements. The midnight plasma cortisol test measures cortisol concentrations in the blood.
Dexamethasone-corticotropin-releasing hormone (CRH) test. Some people have high cortisol levels but do not develop the progressive effects of Cushing’s syndrome, such as muscle weakness, fractures, and thinning of the skin. These people may have pseudo-Cushing’s syndrome, a condition sometimes found in people who have depression or anxiety disorders, drink excess alcohol, have poorly controlled diabetes, or are severely obese. Pseudo-Cushing’s does not have the same long-term effects on health as Cushing’s syndrome and does not require treatment directed at the endocrine glands.
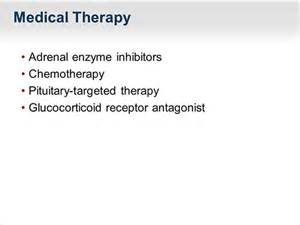
Treatment of Cushings Syndrome:
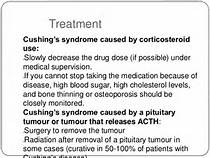
Treatment of cushings syndrome is by castigation of the under lying cause. Treatments for Cushing’s syndrome are contrived to pass your body’s cortisol production to normal. By indurate, or even distinctly lowering cortisol levels, you’ll feel evident improvements in your signs and symptoms. Left untreated, however, Cushing’s syndrome can finally induce to death. The treatment choice depend on the cause. For example:
*If a tumour in an adrenal gland is the reason, an operation to withdraw it will cure the condition.
*For adrenal hyperplasia, both adrenal glands may require to be withdraw. You will then require to take lifelong replacement therapy of several adrenal hormones.
*Other tumours in the body that produce ‘ectopic’ ACTH may be able to be removed, depending on the kind of tumour, where it is, etc.
*Medication to block the production or consequence of cortisol may be a choice.
Ending line treatments for Cushing syndrome are designed to lower the high level of cortisol in your body. The best treatment for you depends on the cause of the syndrome. Treatment options include:
- Reducing corticosteroid use. If the cause of Cushing syndrome is long-term use of corticosteroid medications, your doctor may be able to keep your Cushing signs and symptoms under control by reducing the dosage of the drug over a period of time, while still adequately managing your asthma, arthritis or other condition. For many of these medical problems, your doctor can prescribe noncorticosteroid drugs, which will allow him or her to reduce the dosage or eliminate the use of corticosteroids altogether.
Don’t reduce the dose of corticosteroid drugs or stop taking them on your own. Do so only under your doctor’s supervision.
Abruptly discontinuing these medications could lead to deficient cortisol levels. Slowly tapering off corticosteroid drugs allows your body to resume normal cortisol production.
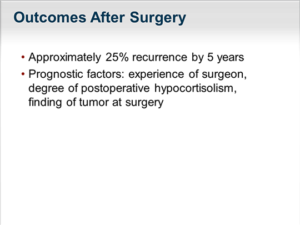
- If the cause of Cushing syndrome is a tumor, your doctor may recommend complete surgical removal. Pituitary tumors are typically removed by a neurosurgeon, who may perform the procedure through your nose. If a tumor is present in the adrenal glands, lungs or pancreas, the surgeon can remove it through a standard operation or in some cases by using minimally invasive surgical techniques, with smaller incisions.
After the operation, you’ll need to take cortisol replacement medications to provide your body with the correct amount of cortisol. In most cases, you’ll eventually experience a return of normal adrenal hormone production, and your doctor can taper off the replacement drugs.
However, this process can take up to a year or longer. In some instances, people with Cushing syndrome never experience a resumption of normal adrenal function; they then need lifelong replacement therapy.
Radiation therapy. If the surgeon can’t totally remove a pituitary tumor, he or she will usually prescribe radiation therapy to be used in conjunction with the operation. Additionally, radiation may be used for people who aren’t suitable candidates for surgery.
Radiation can be given in small doses over a six-week period, or with a technique called stereotactic radiosurgery (Gamma Knife surgery). In the latter procedure, administered as a single treatment, a large dose of radiation is delivered to the tumor, and the radiation exposure to surrounding tissues is minimized.
- Medications can be used to control cortisol production when surgery and radiation don’t work. Medications may also be used before surgery in people who have become very sick with Cushing syndrome. Doctors may recommend drug therapy before surgery to improve signs and symptoms and minimize surgical risk.
Medications to control excessive production of cortisol at the adrenal gland include: ketoconazole (Nizoral), mitotane (Lysodren) and metyrapone (Metopirone).
Mifepristone (Korlym) is approved for people with Cushing syndrome who have type 2 diabetes or glucose intolerance. Mifepristone does not decrease cortisol production, but it blocks the effect of cortisol on your tissues.
Side effects from these medications may include fatigue, nausea, vomiting, headaches, muscle aches, high blood pressure, low potassium and swelling. Some have more serious side effects, such as neurological side effects and liver toxicity.
The newest medication for Cushing’s is pasireotide (Signifor), and it works by decreasing ACTH production from a pituitary tumor. This medication is given as an injection twice daily. It’s recommended if pituitary surgery is unsuccessful or cannot be done.
Side effects are fairly common, and may include diarrhea, nausea, high blood sugar, headache, abdominal pain and fatigue.
In some cases, the tumor or its treatment will cause other hormones produced by the pituitary or adrenal gland to become deficient and your doctor will recommend hormone replacement medications.
If none of these treatment options are appropriate or effective, your doctor may recommend surgical removal of your adrenal glands (bilateral adrenalectomy). This procedure will cure excess production of cortisol, but will require lifelong replacement medications.
Complications are rare with this procedure but could include:
Bruising on your thigh
Ear pain during the procedure
Very rarely, neurological problems
QUOTE FOR TUESDAY:
“Cushing’s syndrome is a hormonal disorder caused by prolonged exposure of the body’s tissues to high levels of the hormone cortisol.”
NIH National Institute of Diabetes and Digestive and Kidney Diseases (U.S. Department of Health and Human Services)
Part II Cushing Syndrome – signs and symptoms in children and adults with complications!
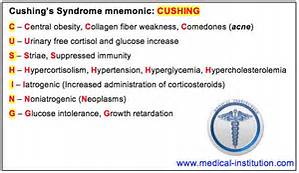
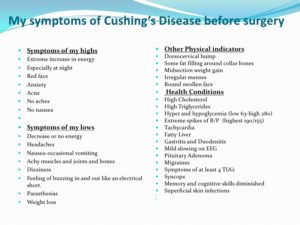
Symptoms of Cushings Syndrome
Symptom of cushings syndrome include fat deposits close to the face neck and trunk; weariness; muscular weakness; salt and water retention; acne; leisurely bruising; menstlruall irregularities; and signs (in women) of virilisation, such as increase of the voice, commute in body, shape, loss of scalp hair, and extend in facial and body hair. Complications of cushings syndrome include advanced blood pressure, The symptoms and signs of cushings syndrome induced by a chronic redundant of corticosteroid hormones in the blood. The redundant may be acquired by a tumour of the outer part (cortex) of the adrenal gland, or may be referable to over inspiration of the adrenal glands by a tumour the pituitary gland.
Many children and teenagers with Cushing’s syndrome will exhibit various symptoms of the following:
-extreme weight gain
-growth retardation
-missed periods in teenage girls
-excess hair growth
-acne
-reddish-blue streaks on the skin
-high blood pressure
-tiredness and weakness
-either very early or late puberty
Adults with the disease may also have symptoms of intense weight gain, redundant hair growth, high blood pressure, and skin difficulties. In addition, they may show:
-muscle and bone weakness
-moodiness, irritability, or depression
-sleep disturbances
-high blood sugar
-menstrual disorders in women and diminished fertility in men
Complications include:
-Diabetes (High or Low blood glucose levels)
-Enlargement of pituitary tumor and other complications from the tumor growth
-Fractures due to osteoporosis which are common in older people
-High blood pressure which could be life threatening
-Kidney stones from the increase in cortisol and other chemicals filtered through the kidneys
-Serious infections which could lead to further secondary infections
Stayed tune for Part III on Cushing’s Disease regarding the diagnosing and treatment of Cushing’s Syndrome.