
Though not all birth defects can be avoided, prenatal care and awareness of past or current conditions can help with prevention.
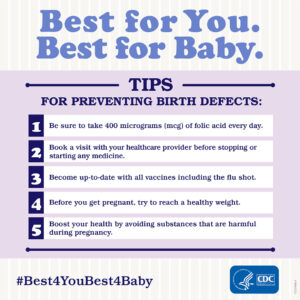
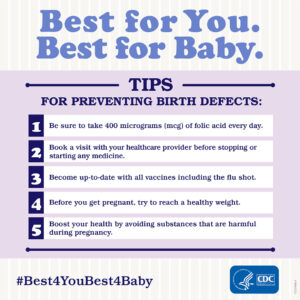
- Prenatal care. Taking a daily prenatal vitamin that includes at least 400 micrograms of folic acid can help prevent a variety of birth defects. You should be taking prenatal vitamins if you’re of reproductive age, when you’re actively trying to conceive and/or as soon as you find out you are pregnant. In addition to taking your prenatal vitamin, avoiding alcohol, tobacco and illegal drugs can significantly help prevent birth defects and pregnancy complications.
- Awareness of past or current conditions. If you previously had a pregnancy with a birth defect, it’s important to find out the most likely causes because it can help your physician plan preventive measures for your next pregnancy. For example, spina bifida is caused by a deficiency in folate, so if your previous pregnancy had spina bifida, you can take a high dose of folate to help prevent future spina bifida diagnoses.
Are all birth defects discovered before a baby is born?
It’s not always possible to detect all birth defects in utero. However, high-resolution ultrasounds done by certified prenatal ultrasound groups make it possible to diagnose defects that will cause a significant impact before birth.
Baschat says: “At the Center for Fetal Therapy, we recommend that pregnant women have the first-trimester nuchal translucency scan between 11 and 14 weeks and the anatomy scan between 18 and 20 weeks. These two ultrasounds provide us with the best opportunity for detecting birth defects.”
In recent years, some pregnant women have turned down the first-trimester ultrasound because a maternal screening blood test now exists for Down syndrome. The ultrasound is still strongly recommended, though, because there are many other serious birth defects that can be detected this early in pregnancy.
Is it possible to treat birth defects while a baby is in utero?
Absolutely. While there are many different types of birth defects, it’s extremely important to try to correct those that damage vital organs before the baby is born. The Center for Fetal Therapy specializes in treating several of these defects in utero, including:
- Congenital diaphragmatic hernia. This condition, in which a hole in the diaphragm allows abdominal content to enter the chest and restrict lung development, can be significantly helped in utero through fetoscopic endotracheal occlusion, a surgery that improves lung function and significantly increases survival rates.
- Lower urinary tract obstruction. This occurs when the flow of urine is blocked from exiting the fetus’ body, leading to permanent kidney damage. Relieving this obstruction before birth protects the kidneys.
Fetal treatments also exist for conditions that make the baby unhealthy, even if they are not considered to be birth defects. For example, if a fetus has an irregular heartbeat, you can give the mother medication that will cross the placenta and treat the fetus.
How successful are in utero treatments for fetal conditions?
By treating fetal conditions in utero rather than waiting until after birth, fetuses are given significantly better chances of survival and a reduced need for major surgery after birth. For example, with a condition like twin-to-twin transfusion syndrome, in which identical twins develop a blood volume imbalance, both babies could die without any intervention. By performing laser surgery in utero, there is approximately a 95 percent chance that at least one baby will survive.
Explains Baschat, “Success rates vary depending on the condition, available treatments and the individual patient, but overall, where fetal interventions are available, we see a much higher rate of survival for affected fetuses.”
If a baby has fetal surgery, will he/she need different care after birth?
This will depend on the individual condition and type of surgery performed. For all fetal surgeries, your baby needs to be delivered at a hospital where pediatric subspecialties are in-house so the baby’s care can be managed after birth. Baschat says: “Many of the treatments we perform require patients to deliver at the highest-level multispecialty hospital, like The Johns Hopkins Hospital. This way, all prenatal and postnatal care is available to you in one location.”
If you have one child affected by a birth defect, will all of your future children have that same condition?
All future children will not definitively be affected by the same birth defect, but it will depend on what the cause was. If the birth defect was caused by a genetic mutation, there may be a higher likelihood of recurrence, but if you seek care from a specialized center, maternal-fetal medicine specialists and genetic counselors can work with you to assess future risk.
The risk of some conditions can be determined before you become pregnant through genetic testing. If that doesn’t exist for the condition in question, maternal-fetal medicine specialists and genetic counselors can genetically test your fetus during pregnancy to see if she or he exhibits the mutation that affected your previous child.
Are there communities in which you can speak with other families who have had children affected by birth defects?
There are many forums online, whether on the web or social media platforms, in which parents come together. “At our center, we reach out to previous patients to see if they are interested in communicating with new patients affected by the same condition,” Baschat explains. “They can empathize about the specific birth defect, but they can also provide guidance and advice about the experience of working with our center throughout the pregnancy and after the baby is born.”
In the future, what advances will take place in treating disease before birth?
Through prenatal diagnosis and understanding fetal disease better, physicians are learning more about what harms the fetus and what may be of benefit before birth. Additionally, new uses for minimally invasive surgical equipment are regularly being discovered.
There are also stem cell therapies, genomic medicine and a whole host of related treatments that are currently used for children and adults. One day, these may also apply to the fetus. “While it’s hard to predict the future, we’re currently doing things we couldn’t have foreseen 10 years ago, so we’re very hopeful for continued advancements in fetal care,” says Baschat.