Harvard Health Publishing states the following:
“If you’d like to cut down your alcohol consumption or start the new year with a clean slate, join in the Dry January challenge by choosing not to drink beer, wine, or spirits for one month. Dry January began in 2012 as a public health initiative from Alcohol Change UK, a British charity. Now millions take part in this health challenge every year.
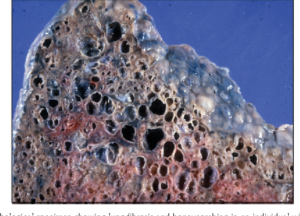
While past observational studies suggested a link between drinking a moderate amount of alcohol and health benefits for some people, more recent research has questioned whether any amount of alcohol improves health outcomes. And heavier drinking or long-term drinking can increase physical and mental problems, especially among older adults. Heart and liver damage, a higher cancer risk, a weakened immune system, memory issues, and mood disorders are common issues.
Yet, cutting out alcohol for even a month can make a noticeable difference in your health. Regular drinkers who abstained from alcohol for 30 days slept better, had more energy, and lost weight, according to a study in BMJ Open. They also lowered their blood pressure and cholesterol levels and reduced cancer-related proteins in their blood.
Tips for a successful Dry January
A month may seem like a long time, but most people can be successful. Still, you may need assistance to stay dry in January. Here are some tips:
- Find a substitute non-alcoholic drink. For social situations, or when you crave a cocktail after a long day, reach for alcohol-free beverages like sparkling water, soda, or mocktails (non-alcoholic cocktails.)
Non-alcoholic beer or wine also is an option, but some brands still contain up to 0.5% alcohol by volume, so check the label. “Sugar is often added to these beverages to improve the taste, so try to choose ones that are low in sugar,” says Dawn Sugarman, a research psychologist at Harvard-affiliated McLean Hospital in the division of alcohol, drugs, and addiction.
- Avoid temptations. Keep alcohol out of your house. When you are invited to someone’s home, bring your non-alcoholic drinks with you.
- Create a support group. Let friends and family know about your intentions and encourage them to keep you accountable. Better yet, enlist someone to do the challenge with you.
- Use the Try Dry app. This free app from the UK helps you track your drinking, set personal goals, and offers motivational information like calories and money saved from not drinking. It’s aimed at cutting back on or cutting out alcohol, depending on your choices.
- Don’t give up. If you slip up, don’t feel guilty. Just begin again the next day.
Check your feelings
Sugarman recommends people also use Dry January to reflect on their drinking habits. It’s common for people to lose their alcohol cravings and realize drinking need not occupy such an ample space in their lives. If this is you, consider continuing for another 30 days, or just embrace your new attitude toward drinking where it’s an occasional indulgence.
If you struggle during the month, or give up after a week or so, you may need extra help cutting back. Talk to your doctor about getting the help you need.
The Rethinking Drinking site created by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) is also an excellent resource. For the record, NIAAA recommends limiting alcohol to two daily drinks or less for men and no more than one drink a day for women.
Be aware of problems that might crop up
Dry January can reveal signs of potential alcohol problems, including symptoms of alcohol withdrawal ranging from mild to serious, depending on how much you usually drink.
- Mild symptoms include anxiety, shaky hands, headache, nausea, vomiting, sweating, and insomnia.
- Severe symptoms often kick in within two or three days after you stop drinking. They can include hallucinations, delirium, racing heart rate, and fever.
“If you suffer alcohol withdrawal symptoms at any time, you should seek immediate medical help,” says Sugarman.”