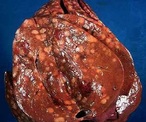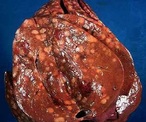


NASH LIVER DISEASED LIVER FATTY TISSUE LIVER
Liver Disease is also referred to Hepatic Disease. Liver Disease is a term that is used when there is any disturbance of the liver function that causes illness. It is a broad term to describe when more than 75% or three quarters of liver tissue needed is affected and decreased function in the liver occurs. The number one cause of liver disease is alcohol abuse in North America. They can cause liver inflammation, referred to as alcoholic hepatitis. Other causes include Cirrhosis, Cholestasis, Steatosis, Hepatitis, Viruses, Non-Alcoholic Fatty Liver, Hemachromatosis, Wilson’s Disease and Gilbert’s Disease.
Causes: Cirrhosis
Cirrhosis is when the liver cells are replaced by permanent scar tissue as a result of chronic liver disease. It is considered the late-stage of liver disease. Cirrhosis is common among chronic alcohol abuse users where the fat accumulation occurs in the liver cells and causes scar tissue. Cholestasis is when the bile flow is obstructed from the gallbladder or duodenum. Steatosis is the term used when cholesterol and triglycerides accumulate in the liver.
Causes: Hepatitis
Hepatitis is a term used to describe the inflammation on liver cells. They can become inflamed due to infection.
There are many forms of Hepatitis:
Hepatitis A (Hep A) is a viral infection primarily spread through the fecal-oral route when small amounts of infected fecal matter are ingested. An acute inflammation of the liver occurs but there is a way to prevent this type of infection. There is a vaccine available and the best way to help prevent it is by a good hand washing.
Hepatitis B (Hep B) is spread by exposure to body fluids and can cause an acute infection. If left untreated, it can progress into a chronic inflammation and on into cirrhosis. There is also a vaccine for this form of hepatitis. Typically, the vaccine contains both Hep A and B in a combination series of doses.
Hepatitis C (Hep C) is caused by a virus different from Hep A or Hep B. It can either be “acute” or “chronic” and is primarily spread through contact with the blood of an infected person. The most common way is by sharing needles or other equipment to inject drugs. Before 1992, Hepatitis C was also commonly spread through blood transfusions and organ transplants which led to the start of a widespread screening of blood supplies. Another way it can be transmitted is through being born to a mother who has it. There are less common ways to contract Hepatitis C, and that’s through sharing personal care items that may have come into contact with another person’s blood (razors, toothbrushes), or having unprotected sex with a infected person. Some people are at an increased risk for Hepatitis C. Those individuals include: Children born to mothers infected with this Hep C; current injection drug users (most common way Hepatitis C is spread in the US), past injection drug users, recipients of donated blood (blood products and organs), hemodialysis patients who spent many years on dialysis for kidney failure, people who received body piercings or tattoos done with non-sterile instruments, & people with known exposure to Hepatitis C like Health care workers or recipients of blood or organs from a donor who tested positive.
Hepatitis D (Hep D) is known as “delta hepatitis” can also be “acute” or “chronic” but is uncommon in the United States. It requires the Hepatitis B virus to survive. It is transmitted through sexual contact with infected blood or blood products. There is also no vaccine available for this virus. Hepatitis E (Hep E) is caused by Ribonucleic Acid (RNA) virus. It is transmitted mainly through the fecal-oral route due to fecal contaminated drinking water.
Causes: NAFLD
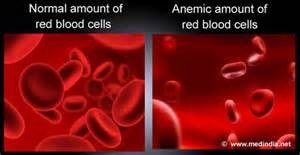
Non-alcoholic fatty liver disease (NAFLD) is the build up of extra fat in liver cells that is not caused by alcohol. It is normal for the liver to contain some fat. liver’s weight is fat, then it NAFLD tends to develop in people who are overweight or obese or have diabetes, high cholesterol or high triglycerides. Rapid weight loss and poor eating habits also may lead to NAFLD. However, some people develop NAFLD even if they do not have any risk factors. NAFLD affects up to 25% of people in the United States. However, if more than 5% up to 10% of the liver’s weight is fat then the liver is called a fatty liver called steatosis. Non-Alcoholic Fatty Liver (NAFL) describes the accumulation of fat within the liver that can cause an inflammation and a gradual decrease in function.
Causes: NAFLD
Those at risk for NAFLD? NAFLD tends to develop in people who are overweight or obese or have diabetes, high cholesterol or high triglycerides. Rapid weight loss and poor eating habits also may lead to NAFLD. However, some people develop NAFLD even if they do not have any risk factors. NAFLD affects up to 25% of people in the United States.
RISKS NAFLD may cause the liver to swell (steatohepatitis). A swollen liver may cause scarring (cirrhosis) over time and may even lead to liver cancer or liver failure.
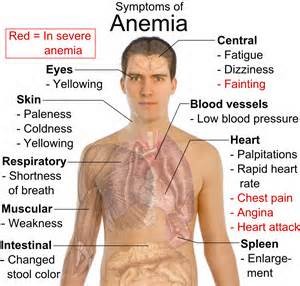
SYMPTOMS NAFLD often has no symptoms. When symptoms occur, they may include fatigue, weakness, weight loss, loss of appetite, nausea, abdominal pain, spider-like blood vessels, yellowing of the skin and eyes (jaundice), itching, fluid build up and swelling of the legs (edema) and abdomen (ascites), and mental confusion.
DIAGNOSIS NAFLD is initially suspected if blood tests show high levels of liver enzymes. However, other liver diseases are first ruled out through additional tests. Often, an ultrasound is used to confirm the NAFLD diagnosis.
TREATMENT There are no medical treatments yet for NAFLD. Eating a healthy diet and exercising regularly may help prevent liver damage from starting or reverse it in the early stages.
- See a doctor who specializes in the liver regularly
- Talk to your doctor about ways to improve your liver health
- Lose weight, if you are overweight or obese
- Lower your cholesterol and triglycerides
- Control your diabetes
- Avoid alcohol
- *
- PREVENTION There are ways to prevent NAFLD:
- Maintain a healthy weight
- Eat a healthy diet
- Exercise regularly
- Limit alcohol intak
- Only take medicines that you need and follow dosing recommendations. The more severe form of NAFLD is called non-alcoholic steatohepatitis (NASH). NASH causes the liver to swell and become damaged. NASH tends to develop in people who are overweight or obese, or have diabetes, high cholesterol or high triglycerides. NASH can occur in many.
- *
- Causes: NASH:Nonalcoholic steatohepatitis or NASH is a common, often “silent” liver disease. It resembles alcoholic liver disease, but occurs in people who drink little or no alcohol. The major feature in NASH is fat in the liver, along with inflammation and damage. Most people with NASH feel well and are not aware that they have a liver problem. Nevertheless, NASH can be severe and can lead to cirrhosis, in which the liver is permanently damaged and scarred and no longer able to work properly.NASH affects 2 to 5 percent of Americans. An additional 10 to 20 percent of Americans have fat in their liver, but no inflammation or liver damage, a condition called “fatty liver.” Although having fat in the liver is not normal, by itself it probably causes little harm or permanent damage. If fat is suspected based on blood test results or scans of the liver, this problem is called nonalcoholic fatty liver disease (NAFLD). If a liver biopsy is performed in this case, it will show that some people have NASH while others have simple fatty liver.
- Most people with NASH are between the ages of 40 and 60 years. It is more common in women than in men. NASH often has no symptoms and people can have NASH for years before symptoms occur. NASH is one of the leading causes of cirrhosis in the United States. Up to 25% of adults with NASH may have cirrhosis. Know people have NASH even if they do not have one risk factor can get the disease.
- Both NASH and NAFLD are becoming more common, possibly because of the greater number of Americans with obesity. In the past 10 years, the rate of obesity has doubled in adults and tripled in children. Obesity also contributes to diabetes and high blood cholesterol, which can further complicate the health of someone with NASH. Diabetes and high blood cholesterol are also becoming more common among Americans.
-
- Nonalcoholic steatohepatitis (NASH) is fat in the liver, with inflammation and damage.
- NASH occurs in people who drink little or no alcohol and affects 2 to 5 percent of Americans, especially people who are middle-aged and overweight or obese.
- NASH can occur in children.
- People who have NASH may feel well and may not know that they have a liver disease.
- NASH can lead to cirrhosis, a condition in which the liver is permanently damaged and cannot work properly.
- Fatigue can occur at any stage of NASH.
- Weight loss and weakness may begin once the disease is advanced or cirrhosis is present.
- NASH may be suspected if blood tests show high levels of liver enzymes or if scans show fatty liver.
- NASH is diagnosed by examining a small piece of the liver taken through a needle, a procedure called biopsy.
- People who have NASH should reduce their weight, eat a balanced diet, engage in physical activity, and avoid alcohol and unnecessary medications.
- No specific therapies for NASH exist. Experimental therapies being studied include antioxidants and antidiabetes medications.
Other Pointers in knowing about the types of liver diseases:
- Most liver diseases are managed and not cured. The exception is for gallstone disease and some viral infections like Hepatitis A and infectious mononucleosis. All forms of liver disease has the ability to progress to cirrhosis and cause liver failure. Complications associated with cirrhosis and liver failure include an increased risk of bleeding and infection, malnutrition and weight loss, and decreased cognitive function.
- Depending on the type of cause for liver disease, determines how it is treated. Hep A requires supportive care from others to maintain hydration while the body’s immune system continues to fight off infections. Other diseases may require long-term care to control and minimize consequences of a particular disease. With cirrhosis and end-stage liver disease patients, they are often given medications to control the amount of protein absorbed in the diet. For other cirrhosis patients, they may not be able to metabolize waste products which raises their blood ammonia levels. To help them function, they need to take water pills (diuretics) and start a low sodium diet to minimize water retention. Only when all other options have failed is liver transplantation an option.
- Symptoms of liver disease range depending on the exact cause for the limited liver function. The general symptoms include a weakness or fatigue, weight loss, nausea, vomiting, fever and a yellow discoloration. If these symptoms are experienced without an explanation, it may be time to consult a medical professional. The time for education is before something like this happens. The survival rate is much higher for the individuals that seek medical attention early on through the act of having the knowledge to make the right decision. By the way the yellow discoloration is what we call Jaundice.
- Some of the other viruses that cause liver disease are viral infections like Mononucleosis, Adenovirus and Cytomegalovirus. There are also non-viral infections like toxoplasmosis and Rocky Mountain Spotted fever that could lead to liver disease but they are less common.
- There are other conditions like Hemachromatosis (iron overload), which is a metabolic disorder that leads to abnormally elevated amounts of iron that is stored in the body. It is an inherited disease. Wilson’s disease is another inherited disease but it affects the body’s ability to metabolize copper. Gilbert’s Disease is an abnormality in bilirubin metabolism in the liver and affects up to 7% of the North American population.
- Most people with NASH are between the ages of 40 and 60 years. It is more common in women than in men. NASH often has no symptoms and people can have NASH for years before symptoms occur. NASH is one of the leading causes of cirrhosis in adults in the United States. Up to 25% of adults with NASH may have cirrhosis. Know people have NASH even if they do not have one risk factor.
Due to alcohol abuse acting as the most common cause of liver disease, it is recommended that alcohol consumption is in moderation. It may help minimize the risk of alcohol-related liver disease. Hepatitis B and C contraction can be decreased by minimizing the risk of exposure to another person’s bodily fluids. There is a vaccination available for Hepatitis A and B. There is screening available for Hepatitis C at most clinics or doctors offices. Fatty liver disease is preventable by the promotion of a healthy lifestyle. Those lifestyle choices include a well-balanced diet, weight control, avoiding excess alcohol consumption and routine exercise.