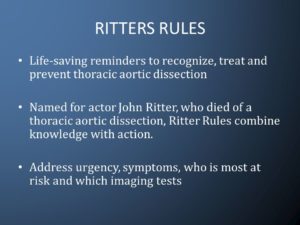
Named for actor John Ritter, who died of a thoracic aortic dissection, Ritter Rules combine knowledge with action. Address urgency, symptoms, who is most at risk and which imaging tests.
Remember that great comedian and actor in our time John Ritter. A man non stop in his work and one day on his set doing doing the show “Eight simple rules for dating my daughter.” when becoming severely perspired, weak to nausea/vomiting than laying down in his trailer. His colleagues knew this was never him and took him to the hospital across the street where he was being treated for a heart attack. After 4 to 5 hours this occurred he was being rushed to the OR to be possibly saved for Aortic Dissection but like many it was too LATE! No one knows they have it till in the hospital and hopefully caught in time. How do you prevent this GO TO A CARDIOLOGIST yearly and be checked after age 50 or much sooner if heredity in the family. Just like so many other diseases, you don’t know till your diagnosed by a doctor that you have it. Some are easier in picking up but this problem is sneaks up behind you and may not be reversible for you, like in Ritter’s case.
What is a thoracic aortic aneurysm?
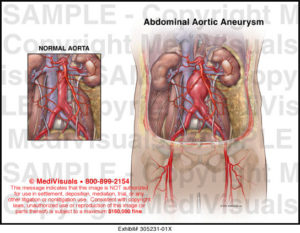
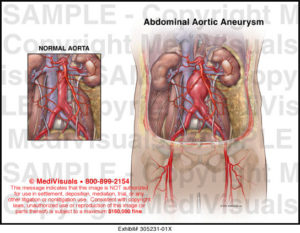
The aorta is the largest blood vessel in the body. It delivers oxygenated blood from the heart to the rest of the body. An aortic aneurysm is a bulging, weakened area in the wall of the aorta. Over time, the blood vessel balloons and is at risk for bursting (rupture) or separating (dissection). This can cause life threatening bleeding and potentially death.
“Thoracic” refers to the part of the aorta that runs through the chest (thoracic aortic aneurysm). Aneurysms occur more often in the portion of the aorta that runs through the abdomen (abdominal aortic aneurysm).
Once formed, an aneurysm will gradually increase in size and get progressively weaker.
Thoracic Aortic Aneurysm and Aortic Dissection describe forms of aortic disease. When the walls of a section of blood vessel become weak and thin, it results in a bulging or ballooning of the vessel that is commonly called an aneurysm (like a thin punching bag). Dissection is the tearing of a blood vessel’s inner lining, causing blood to leak between the layers of the vessel wall and blood only for so long can bleed between those layers till the obvious. An aneurysm may tear (dissect) or completely rupture that area of the aorta. Under certain conditions, a blood vessel may dissect even when there is no aneurysm.
When the aneurysm and/or dissection involve the aorta (the main artery leading away from the heart), the bulging and tearing are considered among the most serious, life-threatening conditions. However, the diseased aorta can be successfully treated, especially when found before an emergency occurs. The US National Center for Health Statistics reports almost 15,000 aorta-related deaths (including both the thoracic and abdominal aorta) each year.
What are the symptoms of a thoracic aortic aneurysm?
Thoracic aortic aneurysms may not cause symptoms. When symptoms do occur, they may be related to the location, size, and how fast the aneurysm is growing.
Sudden, severe pain associated with a thoracic aneurysm may be a sign of a life-threatening medical emergency.
Symptoms of a thoracic aneurysm may include:
-
Pain in the jaw, neck, or upper back-This is why the ER is thinking its a heart attack.
-
Pain in the chest or back-This is why the ER is thinking its a heart attack.
-
Wheezing, coughing, or shortness of breath as a result of pressure on the trachea (windpipe)
-
Hoarseness as a result of pressure on the vocal cords
-
Trouble swallowing due to pressure on the esophagus
The symptoms of a thoracic aortic aneurysm may look like other conditions. See your doctor for a diagnosis.
How is a thoracic aortic aneurysm diagnosed?
Your doctor will do a complete medical history and physical exam. Other possible tests include:
-
Computed tomography scan (also called a CT or CAT scan). This test uses X-rays and computer technology to make horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than standard X-rays.
-
Magnetic resonance imaging (MRI). This test uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body.
-
Echocardiogram (also called echo). This test evaluates the structure and function of the heart by using sound waves recorded on an electronic sensor that make a moving picture of the heart and heart valves, as well as the structures within the chest, such as the lungs and the area around the lungs and the chest organs.
-
Transesophageal echocardiogram (TEE). This test uses echocardiography to check for aneurysm, the condition of heart valves, or presence of a tear of the lining of the aorta. TEE is done by inserting a probe with a transducer on the end down the throat.
-
Chest X-ray. This test uses invisible electromagnetic energy beams to make images of internal tissues, bones, and organs onto film.
-
Arteriogram (angiogram). This is an X-ray image of the blood vessels that is used to assess conditions such as aneurysm, narrowing of the blood vessel, or blockages. A dye (contrast) will be injected through a thin, flexible tube placed in an artery. The dye makes the blood vessels visible on an X-ray.
What is the treatment for thoracic aortic aneurysm?
Treatment may include:
-
Monitoring with MRI or CT. These tests are done to check the size and rate of growth of the aneurysm.
-
Managing risk factors. Steps, such as quitting smoking, controlling blood sugar if you have diabetes, losing weight if overweight, and eating a healthy diet may help control the progression of the aneurysm. Reversing these problems always helps, doesn’t cure it.
-
Medicine. Used to control factors such as high cholesterol or high blood pressure. These medications doing this control of conditions listed helps keep it from getting worse with pt following up with being checked as M.D. prescribes.
-
Surgery Treatment for a thoracic aneurysm may include surgical repair or removal of the aneurysm, or inserting a metal mesh coil (stent) to support the blood vessel and prevent rupture.
-
Thoracic aortic aneurysm open repair. The type of surgery will depend on the location and type of aneurysm, and your overall health. For an ascending or aortic arch aneurysm, a large incision may be made through the breastbone. If an ascending aneurysm involves damage to the aortic valve of the heart, the valve may be repaired or replaced during the procedure. For a descending aneurysm, a large incision may extend from the back under the shoulder blade around the side of the rib cage to just under the breast. This lets the surgeon to see the aorta directly to repair the aneurysm.
-
Endovascular aneurysm repair (EVAR). EVAR requires only small incisions in the groin. Using X-ray guidance and specially-designed instruments, the surgeon can repair the aneurysm by inserting a metal mesh coil, called a stent-graft, inside the aorta. Not all thoracic aneurysms can be repaired by means of EVAR.
A small aneurysm or one that doesn’t cause symptoms may not require surgical treatment until it reaches a certain size or is rapidly increasing in size over a short period of time. Your doctor may recommend “watchful waiting.” This may include a CT scan or MRI scan every 6 months to closely monitor the aneurysm, and blood pressure medicine may be used to control high blood pressure.
Your doctor may recommend surgery if the aneurysm is causing symptoms or is large.
What is aortic dissection?
An aortic dissection starts with a tear in the inner layer of the aortic wall of the thoracic aorta. The aortic wall is made up of 3 layers of tissue. When a tear occurs in the innermost layer of the aortic wall, blood is then channeled into the wall of the aorta separating the layers of tissues. This generates a weakening in the aortic wall with a potential for rupture. Aortic dissection can be a life-threatening emergency, like in John Ritter’s situation Sept 11, 2003 which led him to death in the ER and attempt to save him in the OR but too late (Died at 54 y/o. missing his next birthday Sept 17). The most commonly reported symptom of an acute aortic dissection is severe, constant chest or upper back pain, sometimes described as “ripping” or “tearing.” The pain may move from one place to another.
When a diagnosis of aortic dissection is confirmed, immediate surgery or stenting is usually done.
For a thoracic aneurysm may include surgical repair or removal of the aneurysm, or inserting a metal mesh coil (stent) to support the blood vessel and prevent rupture. If not treated the vessel continues to weaken getting thinner.
PREVENTION is the key = seeing your cardiologist every 6 months to yearly not for anything overlooked by the expert on our engine of the body (the heart) and diseases of cardiology. Go to the expert over a general doctor so nothing is missed!