Risk factors”
There are only a few known risk factors for narcolepsy, including:
- Age. Narcolepsy typically begins between ages 10 and 30.
- Family history. Your risk of narcolepsy is 20 to 40 times higher if you have a close family member who has it.
Complications:
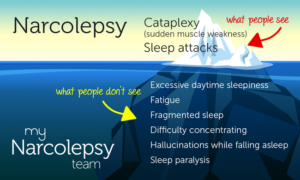
- Public misconception of the condition. Narcolepsy can cause problems at work or in your personal life. Your performance may suffer at school or work. Others might see people with narcolepsy as lazy or lethargic.
- Effects on intimate relationships. Intense feelings, such as anger or joy, can trigger cataplexy. This can cause people with narcolepsy to withdraw from emotional interactions.
- Physical harm. Falling asleep suddenly may result in injury. You’re at increased risk of a car accident if you fall asleep while driving. Your risk of cuts and burns is greater if you fall asleep while cooking.
- Obesity. People with narcolepsy are more likely to be overweight. Sometimes weight rapidly increases when sleepiness symptoms start.
How your MD comes to this Diagnosis:
Your health care provider may suspect narcolepsy based on your symptoms of excessive daytime sleepiness and sudden loss of muscle tone, known as cataplexy. Your provider will likely refer you to a sleep specialist. Formal diagnosis requires staying overnight at a sleep center for an in-depth sleep analysis.
A sleep specialist will likely diagnose narcolepsy and determine how severe it is based on:
- Your sleep history. A detailed sleep history can help with a diagnosis. You’ll likely fill out the Epworth Sleepiness Scale. The scale uses short questions to measure your degree of sleepiness. You’ll answer how likely it is that you would fall asleep in certain times, such as sitting down after lunch.
- Your sleep records. You may be asked to write down your sleep pattern for a week or two. This allows your provider to compare how your sleep pattern may relate to how alert you feel.Your health care provider also may ask you to wear an actigraph. This device is worn like a watch. It measures periods of activity and rest. It provides an indirect measure of how and when you sleep.
- A sleep study, known as polysomnography. This test measures signals during sleep using flat metal discs called electrodes placed on your scalp. For this test, you must spend a night at a medical facility. The test measures your brain waves, heart rate and breathing. It also records your leg and eye movements.
- Multiple sleep latency test. This test measures how long it takes you to fall asleep during the day. You’ll be asked to take four or five naps at a sleep center. Each nap needs to be two hours apart. Specialists will observe your sleep patterns. People who have narcolepsy fall asleep easily and enter into rapid eye movement (REM) sleep quickly.
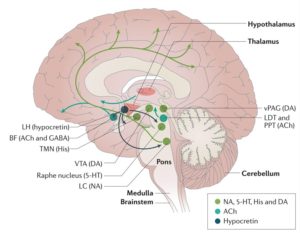
- Genetic tests and a lumbar puncture, known as a spinal tap. Occasionally, a genetic test may be performed to see if you’re at risk of type 1 narcolepsy. If so, your sleep specialist may recommend a lumbar puncture to check the level of hypocretin in your spinal fluid. This test is only done in specialized centers.
These tests also can help rule out other possible causes of your symptoms. Excessive daytime sleepiness could also be caused by sleep deprivation, the use of sedating medicines and sleep apnea.
Treatment:
There is no cure for narcolepsy, but medicines and lifestyle changes can help you manage the symptoms.
Medications
Medicines for narcolepsy include:
- Stimulants. Drugs that stimulate the central nervous system are the primary treatment to help people with narcolepsy stay awake during the day. Your health care provider may recommend modafinil (Provigil) or armodafinil (Nuvigil). These medicines aren’t as habit-forming as older stimulants. They also don’t produce the highs and lows associated with older stimulants. Side effects are uncommon but may include headache, nausea or anxiety.Solriamfetol (Sunosi) and pitolisant (Wakix) are newer stimulants used for narcolepsy. Pitolisant also may be helpful for cataplexy.Some people need treatment with methylphenidate (Ritalin, Concerta, others) or amphetamines (Adderall XR 10, Dexedrine, others). These medicines are effective but can be habit-forming. They may cause side effects such as nervousness and a fast heartbeat.
- Serotonin and norepinephrine reuptake inhibitors (SNRIs) or selective serotonin reuptake inhibitors (SSRIs). These medicines suppress REM sleep. Health care providers prescribe these medicines to help ease the symptoms of cataplexy, hallucinations and sleep paralysis.They include venlafaxine (Effexor XR), fluoxetine (Prozac) and sertraline (Zoloft). Side effects can include weight gain, insomnia and digestive problems.
- Tricyclic antidepressants. These older antidepressants can treat cataplexy. But they can cause side effects such as dry mouth and lightheadedness. These medicines include protriptyline, imipramine (Tofranil) and clomipramine (Anafranil).
- Sodium oxybate (Xyrem) and oxybate salts (Xywav). These medicines work well at relieving cataplexy. They help improve nighttime sleep, which is often poor in narcolepsy. They also may help control daytime sleepiness. It’s taken in two doses, one at bedtime and one up to four hours later.Xywav is a newer formulation with less sodium.These medicines can have side effects, such as nausea, bed-wetting and sleepwalking. Taking them together with other sleeping tablets, narcotic pain relievers or alcohol can lead to trouble breathing, coma and death.
If you take medicines for other health problems, ask your health care provider how they may interact with narcolepsy medicines.
Certain medicines that you can buy without a prescription can cause drowsiness. They include allergy and cold medicines. If you have narcolepsy, your doctor may recommend that you don’t take these medicines.
Researchers are studying other potential treatments for narcolepsy. Medicines being studied include those that target the hypocretin chemical system. Researchers also are studying immunotherapy. Further research is needed before these medicines become available.
Other recommendations with treatment seeing a doctor specializing are:
Lifestyle and home remedies (check with you MD):
Lifestyle changes are important in managing the symptoms of narcolepsy. You may benefit if you:
- Stick to a schedule. Go to sleep and wake up at the same time every day, including weekends.
- Take naps. Schedule short naps at regular intervals during the day. Naps of 20 minutes during the day may be refreshing. They also may reduce sleepiness for 1 to 3 hours. Some people may need longer naps.
- Avoid nicotine and alcohol. Using these substances, especially at night, can worsen your symptoms.
- Get regular exercise. Plan for moderate, regular exercise at least 4 to 5 hours before bedtime. It may help you sleep better at night and feel more awake during the day.
Coping and support
Dealing with narcolepsy can be a challenge. Consider these tips:
- Talk about it. Tell your employer or teachers about your condition. Then work with them to find ways to adjust to your needs. This may include taking naps during the day. Or you might break up repetitive tasks. You might record meetings or classes to refer to later. You also might find it helps to stand during meetings or lectures, and to take brisk walks during the day.The Americans with Disabilities Act prohibits discrimination against workers with narcolepsy. Employers are required to provide reasonable accommodation to qualified employees.
- Be safe while driving. If you must drive a long distance, work with your health care provider to find ways to make a safe trip. Create a medicine schedule that is most likely to keep you awake during your drive. Stop for naps and exercise breaks whenever you feel drowsy. Don’t drive if you feel too sleepy. Better don’t drive at all. Check with your MD first recommended!
Support groups and counseling can help you and your loved ones cope with narcolepsy. Ask your health care provider to help you locate a group or qualified counselor in your area.
Check out doxins with narcolepsy on youtube or facebook!