Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of the Congo (DRC) during a period of intensified effort to eliminate smallpox. Since then, monkeypox has been reported in people in several other central and western African countries: Cameroon, Central African Republic, Cote d’Ivoire, Democratic Republic of the Congo, Gabon, Liberia, Nigeria, Republic of the Congo, and Sierra Leone. The majority of infections are in Democratic Republic of the Congo.
There are two distinct genetic clades of the monkeypox virus – the Central African (Congo Basin) clade and the West African clade. The Congo Basin clade has historically caused more severe disease and was thought to be more transmissible. The geographical division between the two clades has so far been in Cameroon – the only country where both virus clades have been found.
Monkeypox is a viral zoonosis (a virus transmitted to humans from animals) with symptoms very similar to those seen in the past in smallpox patients, although it is clinically less severe. Monkeypox virus is an enveloped double-stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family. With the eradication of smallpox in 1980 and subsequent cessation of smallpox vaccination, monkeypox has emerged as the most important orthopoxvirus for public health. Monkeypox primarily occurs in Central and West Africa, often in proximity to tropical rainforests and has been increasingly appearing in urban areas. Animal hosts include a range of rodents and non-human primates.
Various animal species have been identified as susceptible to monkeypox virus.. This includes rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates and other species. Uncertainty remains on the natural history of monkeypox virus and further studies are needed to identify the exact reservoir(s) and how virus circulation is maintained in nature.
Monkeypox cases in people have occurred outside of Africa linked to international travel or imported animals, including cases in the United States, as well as Israel, Singapore, and the United Kingdom.
The natural reservoir of monkeypox remains unknown. However, African rodents and non-human primates (like monkeys) may harbor the virus and infect people.
Symptoms of Monkey Pox:
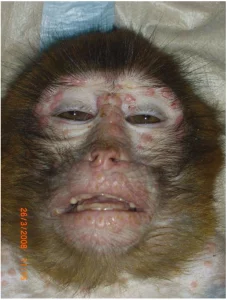
People with monkeypox get a rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus (butthole) and could be on other areas like the hands, feet, chest, face, or mouth.
- The rash will go through several stages, including scabs, before healing.
- The rash can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of monkeypox can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
Monkeypox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
A person with monkeypox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. Some people have been found to have infection but no symptoms. To date, however, there is no evidence that monkeypox spreads from people with no symptoms. CDC will continue to monitor for new or changing information about transmission.
Monkeypox can more accurately be described as “sexually transmissible.” In other words, sex is just one of the ways that monkeypox can be spread. In the past, monkeypox outbreaks have been linked to direct exposure to infected animals and animal products, with limited person-to-person spread. In the current monkeypox outbreak, the virus is spreading primarily through close personal contact. This may include contact with infectious lesions or respiratory secretions via close, sustained skin-to-skin contact that occurs during sex. However, any close, sustained skin-to-skin contact with someone who has monkeypox can spread the virus. The contact does not have to be exclusively intimate or sexual.
Monkeypox can spread from person to person through direct contact with the infectious rash, scabs, or body fluids. It also can be spread by respiratory secretions during prolonged, face-to-face contact, or during intimate physical contact, such as kissing, cuddling, or sex.
A person with monkeypox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. Some people have been found to have infection but no symptoms. To date, however, there is no evidence that monkeypox spreads from people with no symptoms. CDC will continue to monitor for new or changing information about transmission.
When to get tested:
- Currently, testing is only recommended if you have a rash consistent with monkeypox.
- If you think you have monkeypox or have had close personal contact with someone who has monkeypox, consider taking precautions and visit a healthcare provider to help you decide if you need to be tested for monkeypox.
How its diagnosed:
- You will likely need to fill out paperwork before you get tested.
- To get a specimen to test, the healthcare provider will use a swab to rub vigorously across lesions of your rash. They will take swabs from more than one lesion.
- This swabbing may be uncomfortable but is necessary to get enough material to detect the monkeypox virus from the specimens.
- The specimens will be tested in a lab to see if the monkeypox virus is detected.
- Results are usually available within a few days.
- While you are waiting for your results, take precautions to avoid getting or spreading monkeypox virus to others.
The CDC states there is no treatment specifically for monkeypox. But because the viruses that cause monkeypox and smallpox are similar, antiviral drugs developed to protect against smallpox may be used to treat monkeypox effectively.” At at this time there’s currently not an approved antiviral treatment for monkeypox. Monkeypox is usually a self-limited disease with symptoms lasting from two weeks to four weeks.
Most people with monkeypox get better on their own without treatment. Following diagnosis, your healthcare provider will monitor your condition and try to relieve your symptoms like preventing dehydration and give you antibiotics to treat secondary bacterial infections if they develop.
The CDC states “Two vaccines may be used for the prevention of monkeypox disease:
- JYNNEOS vaccine is approved for the prevention of monkeypox and smallpox. During the current outbreak, JYNNEOS is the main vaccine being used in the United States.
- ACAM2000 vaccine is approved for immunization against smallpox and made available for use against monkeypox under an Expanded Access Investigational New Drug (EA-IND) protocol.
- People may be vaccinated after exposure to monkeypox virus to help prevent monkeypox disease (i.e., post-exposure prophylaxis).
- No data are currently available on the clinical efficacy or effectiveness of JYNNEOS or ACAM2000 for monkeypox disease.”
The CDC states “As of November 29, 2022 The total U.S. cases are 29, 325 and the total deaths in the U.S. 15.”