Pulmonary embolism (PULL-mun-ary EM-bo-lizm), or PE, is a sudden blockage in a lung artery. The blockage usually is caused by a blood clot that travels to the lung from a vein in the leg. The clot gets to the right side of the heart and goes into the upper chamber (atrium) down to the lower chamber (ventricles) to the pulmonary artery bringing the clot into the lungs.
A clot that forms in one part of the body and travels in the bloodstream to another part of the body is called an embolus (EM-bo-lus).
PE is a serious condition that can:
- Damage part of your lung because of a lack of blood flow to your lung tissue. This damage may lead to pulmonary hypertension (increased pressure in the pulmonary arteries).
- Cause low oxygen levels in your blood.
- Damage other organs in your body because of a lack of oxygen.
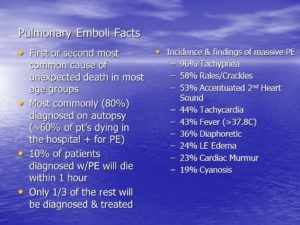
If a blood clot is large, or if there are many clots, PE can cause death.
Overview
PE most often is a complication of a condition called deep vein thrombosis (DVT). In DVT, blood clots form in the deep veins of the body—most often in the legs. These clots can break free, travel through the bloodstream to the lungs, and block an artery.
Deep vein clots are not like clots in veins close to the skin’s surface. Those clots remain in place and do not cause PE.
Outlook
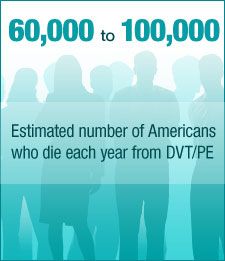
The exact number of people affected by DVT and PE isn’t known. Estimates suggest these conditions affect 300,000 to 600,000 people in the United States each year.
If left untreated, about 30 percent of patients who have PE will die. Most of those who die do so within the first few hours of the event.
The good news is that a prompt diagnosis and proper treatment can save lives and help prevent the complications of PE.
Other Names for Pulmonary Embolism
- Venous thromboembolism (VTE). This term is used for both pulmonary embolism and deep vein thrombosis.
What Causes Pulmonary Embolism?
Major Causes
Pulmonary embolism (PE) usually begins as a blood clot in a deep vein of the leg. This condition is called deep vein thrombosis. The clot can break free, travel through the bloodstream to the lungs, and block an artery.
Blood clots can form in the deep veins of the legs if blood flow is restricted and slows down. This can happen if you don’t move around for long periods, such as:
- After some types of surgery
- During a long trip in a car or airplane
- If you must stay in bed for an extended time
Blood clots are more likely to develop in veins damaged from surgery or injured in other ways.
Other Causes
Rarely, an air bubble, part of a tumor, or other tissue travels to the lungs and causes PE. Also, if a large bone in the body (such as the thigh bone) breaks, fat from the bone marrow can travel through the blood. If the fat reaches the lungs, it can cause PE.
Who Is at Risk for Pulmonary Embolism?
Pulmonary embolism (PE) occurs equally in men and women. The risk increases with age. For every 10 years after age 60, the risk of having PE doubles.
Certain inherited conditions, such as factor V Leiden, increase the risk of blood clotting and PE.
Major Risk Factors
Your risk for PE is high if you have deep vein thrombosis (DVT) or a history of DVT. In DVT, blood clots form in the deep veins of the body—most often in the legs. These clots can break free, travel through the bloodstream to the lungs, and block an artery.
Your risk for PE also is high if you’ve had the condition before.
Other Risk Factors
Other factors also can increase the risk for PE, such as:
- Being bedridden or unable to move around much
- Having surgery or breaking a bone (the risk goes up in the weeks following the surgery or injury)
- Having certain diseases or conditions, such as a stroke, paralysis (an inability to move), chronic heart disease, or high blood pressure
- Smoking
People who have recently been treated for cancer or who have a central venous catheter are more likely to develop DVT, which increases their risk for PE. A central venous catheter is a tube placed in a vein to allow easy access to the bloodstream for medical treatment. A clot can form at the end of it but usually in preventing this if not heparin bolus (ex.300 U in 5 cc of normal saline) is flushed in the catheter if not just flushing the catheter with 10cc of normal saline the prevent the clot forming every 8 hrs or 12 hrs.
Other risk factors for DVT include sitting for long periods (such as during long car or airplane rides), pregnancy and the 6-week period after pregnancy, and being overweight or obese. Women who take hormone therapy pills or birth control pills also are at increased risk for DVT.
The risk of developing blood clots increases as your number of risk factors increases.
What Are the Signs and Symptoms of Pulmonary Embolism?
Major Signs and Symptoms
Signs and symptoms of pulmonary embolism (PE) include unexplained shortness of breath, problems breathing, chest pain, coughing, or coughing up blood. An arrhythmia (irregular heartbeat) also may suggest that you have PE.
Sometimes the only signs and symptoms are related to deep vein thrombosis (DVT). These include swelling of the leg or along a vein in the leg, pain or tenderness in the leg, a feeling of increased warmth in the area of the leg that’s swollen or tender, and red or discolored skin on the affected leg.
See your doctor right away if you have any signs or symptoms of PE or DVT. It’s also possible to have PE and not have any signs or symptoms.
Other Signs and Symptoms
Some people who have PE have feelings of anxiety or dread, light-headedness or fainting, rapid breathing, sweating, or an increased heart rate.
How Is Pulmonary Embolism Diagnosed?
Pulmonary embolism (PE) is diagnosed based on your medical history, a physical exam, and test results.
Doctors who treat patients in the emergency room often are the ones to diagnose PE with the help of a radiologist. A radiologist is a doctor who deals with x rays and other similar tests.
Medical History and Physical Exam
To diagnose PE, the doctor will ask about your medical history. He or she will want to:
- Find out your deep vein thrombosis (DVT) and PE risk factors
- See how likely it is that you could have PE
- Rule out other possible causes for your symptoms
Your doctor also will do a physical exam. During the exam, he or she will check your legs for signs of DVT. He or she also will check your blood pressure and your heart and lungs.
Diagnostic Tests
Many tests can help diagnose PE. Which tests you have will depend on how you feel when you get to the hospital, your risk factors, available testing options, and other conditions you could possibly have. You may have one or more of the following tests.
Ultrasound
Doctors can use ultrasound to look for blood clots in your legs. Ultrasound uses sound waves to check blood flow in your veins.
For this test, gel is put on the skin of your legs. A hand-held device called a transducer is moved back and forth over the affected areas. The transducer gives off ultrasound waves and detects their echoes as they bounce off the vein walls and blood cells.
A computer turns the echoes into a picture on a computer screen, allowing the doctor to see blood flow in your legs. If the doctor finds blood clots in the deep veins of your legs, he or she will recommend treatment.
DVT and PE both are treated with the same medicines.
Computed Tomography Scans
Doctors can use computed tomography (to-MOG-rah-fee) scans, or CT scans, to look for blood clots in the lungs and legs.
For this test, dye is injected into a vein in your arm. The dye makes the blood vessels in your lungs and legs show up on x-ray images. You’ll lie on a table, and an x-ray tube will rotate around you. The tube will take pictures from many angles.
This test allows doctors to detect most cases of PE. The test only takes a few minutes. Results are available shortly after the scan is done.
Lung Ventilation/Perfusion Scan
A lung ventilation/perfusion scan, or VQ scan, uses a radioactive substance to show how well oxygen and blood are flowing to all areas of your lungs. This test can help detect PE.
Pulmonary Angiography
Pulmonary angiography (an-jee-OG-rah-fee) is another test used to diagnose PE. This test isn’t available at all hospitals, and a trained specialist must do the test.
For this test, a flexible tube called a catheter is threaded through the groin (upper thigh) or arm to the blood vessels in the lungs. Dye is injected into the blood vessels through the catheter.
X-ray pictures are taken to show blood flowing through the blood vessels in the lungs. If a blood clot is found, your doctor may use the catheter to remove it or deliver medicine to dissolve it.
Blood Tests
Certain blood tests may help your doctor find out whether you’re likely to have PE.
A D-dimer test measures a substance in the blood that’s released when a blood clot breaks down. High levels of the substance may mean a clot is present. If your test is normal and you have few risk factors, PE isn’t likely.
Other blood tests check for inherited disorders that cause blood clots. Blood tests also can measure the amount of oxygen and carbon dioxide in your blood. A clot in a blood vessel in your lungs may lower the level of oxygen in your blood.
Other Tests
To rule out other possible causes of your symptoms, your doctor may use one or more of the following tests.
- Echocardiography (echo). This test uses sound waves to create a moving picture of your heart. Doctors use echo to check heart function and detect blood clots inside the heart.
- EKG (electrocardiogram). An EKG is a simple, painless test that detects and records the heart’s electrical activity.
- Chest x ray. This test creates pictures of your lungs, heart, large arteries, ribs, and diaphragm (the muscle below your lungs).
- Chest MRI (magnetic resonance imaging). This test uses radio waves and magnetic fields to create pictures of organs and structures inside the body. MRI often can provide more information than an x ray.
How Is Pulmonary Embolism Treated?
Pulmonary embolism (PE) is treated with medicines, procedures, and other therapies. The main goals of treating PE are to stop the blood clot from getting bigger and keep new clots from forming.
Treatment may include medicines to thin the blood and slow its ability to clot. If your symptoms are life threatening, your doctor may give you medicine to quickly dissolve the clot. Rarely, your doctor may use surgery or another procedure to remove the clot.
Medicines
Anticoagulants (AN-te-ko-AG-u-lants), or blood thinners, decrease your blood’s ability to clot. They’re used to stop blood clots from getting larger and prevent clots from forming. Blood thinners don’t break up blood clots that have already formed. (The body dissolves most clots with time.)
You can take blood thinners as either a pill, an injection, or through a needle or tube inserted into a vein (called intravenous, or IV, injection). Warfarin is given as a pill. (Coumadin® is a common brand name for warfarin.) Heparin is given as an injection or through an IV tube; usually given as Heparin drip than when Counmadin starts within 24 hrs the drip is discontinued in the hospital and the patient stays on coumadin or some type of blood thinner as the MD prescribes.
At times, your doctor may treat you with both heparin and warfarin at the same time. Heparin acts quickly. Warfarin takes 2 to 3 days before it starts to work. Once warfarin starts to work, heparin usually is stopped.
Pregnant women usually are treated with heparin only, because warfarin is dangerous for the pregnancy.
If you have deep vein thrombosis, treatment with blood thinners usually lasts for 3 to 6 months. If you’ve had blood clots before, you may need a longer period of treatment. If you’re being treated for another illness, such as cancer, you may need to take blood thinners as long as PE risk factors are present.
The most common side effect of blood thinners is bleeding. This can happen if the medicine thins your blood too much. This side effect can be life threatening.
Sometimes the bleeding is internal, which is why people treated with blood thinners usually have routine blood tests. These tests, called PT and PTT tests, measure the blood’s ability to clot. These tests also help your doctor make sure you’re taking the right amount of medicine. Call your doctor right away if you’re bruising or bleeding easily.
Thrombin inhibitors are a newer type of blood-thinning medicine. They’re used to treat some types of blood clots in people who can’t take heparin.
Emergency Treatment
When PE is life threatening, a doctor may use treatments that remove or break up the blood clot. These treatments are given in an emergency room or hospital.
Thrombolytics (THROM-bo-LIT-iks) are medicines that can quickly dissolve a blood clot. They’re used to treat large clots that cause severe symptoms. Because thrombolytics can cause sudden bleeding, they’re used only in life-threatening situations.
Sometimes a doctor may use a catheter (a flexible tube) to reach the blood clot. The catheter is inserted into a vein in the groin (upper thigh) or arm and threaded to the clot in the lung. The doctor may use the catheter to remove the clot or deliver medicine to dissolve it.
Rarely, surgery may be needed to remove the blood clot.
Other Types of Treatment
If you can’t take medicines to thin your blood, or if the medicines don’t work, your doctor may suggest a vena cava filter. This device keeps blood clots from traveling to your lungs.
The filter is inserted inside a large vein called the inferior vena cava. (This vein carries blood from the body back to the heart). The filter catches clots before they travel to the lungs. This type of treatment can prevent PE, but it won’t stop other blood clots from forming.
Graduated compression stockings can reduce the chronic (ongoing) swelling that a blood clot in the leg may cause.
Graduated compression stockings are worn on the legs from the arch of the foot to just above or below the knee. These stockings are tight at the ankle and become looser as they go up the leg. This causes gentle compression (pressure) up the leg. The pressure keeps blood from pooling and clotting.