Burn Prevention and Burn Treatment for Kids
Many people have, or know someone who has, a story about learning the concept of ‘hot’ as a child through getting burned. 300 children ages 0-19 are treated in emergency rooms every day for injuries related to burns. Increased public awareness about burns has helped to lower the number of injuries and fatalities caused by burns, scalding, and fires – which is the intent and the importance of Burn Awareness Week. This week, we want to bring awareness to some of the most common ways that children get burned, and how parents and caregivers can aid in burn prevention.
TYPES OF BURNING WITH HOW TO PREVENT THEM:
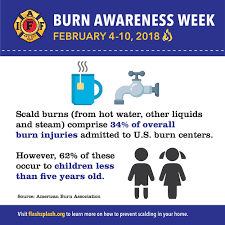
A scald is a burn sustained from a hot liquid or steam. Younger children are most likely to be burned in this way, though anyone can be scalded. To prevent scalding, follow these tips:
- Set your hot water heater to 120℉ or lower. These temperatures should prevent tap water from getting hot enough to burn.
- Always check the temperature of bathwater before placing your child in the bathtub, and never leave your child unattended in the bathroom. Unattended children may accidentally turn on the hot water or increase the temperature, increasing the risk of scalding.
- Set a child-free zone around stoves or hot items in the kitchen until children are old enough to understand the dangers of cooking. Depending on your space and children, this may mean making the kitchen off-limits while cooking, or placing tape on the floor to create a visual barrier for children.
- Turn pot handles toward the back of the stove to prevent them being grabbed, knocked, or pulled off the stovetop.
- Avoid the use of tablecloths with younger children, to prevent them being pulled off the table and bringing hot liquids or cookware with them. Never leave a container (cup, bowl, etc.) with hot liquid at the edge of a table or countertop, in reach of a child.
Cooking is the top cause of fires and burns in homes and should be a focus for burn prevention. Older children are more likely to receive burns from flame or hot objects than scalds. When cooking, make sure to follow these tips to prevent burns in children and adults:
- Never leave the stove on and unattended. This seems logical, but is a common occurrence.
- When using a microwave, make sure to stir foods and always test the temperature. Microwaves do not heat food evenly, leaving some portions hotter than others. Never heat formula or milk in a microwave, for this same reason.
- Do not hold children while cooking, removing food from the stove or microwave, or carrying hot food or liquids.
- When using a grill, smoker, or barbeque, make sure that children play away from the grill and understand that it is hot and will remain that way for many hours.
- Teach older children how to cook safely, providing them age-appropriate cooking tasks.
- Keep children a safe distance from hot oil and frying foods, and utilize a pot lid or splash guard to prevent burns from grease splatter.
While the most common, cooking is not the only way people experience burns. There are many items in the home that can cause burns – some more obvious than others. Here are some additional tips to help prevent burns in other parts of the house:
- Check electrical cords and outlets frequently for wear, fraying, or other damage that could result in heat or fire. Damage to cords can impair their heat retention, causing them to become hot enough to burn or catch nearby materials on fire.
- Make sure you are not overloading electrical outlets or power strips. Too much electricity running through cords or outlets can cause them to become hot, causing burns, melting plastic, or fires. If outlets or power strips are hot to the touch, plugs need to be moved to different outlets to prevent overloading.
- Check heating devices, like space heaters, to ensure they are working properly and make sure to keep them out of reach of children.
- If your home has a fireplace, make sure it is cleaned before you use it and don’t allow children to play on or around it.
- Teach children about heat, fires, and fire safety, including not to play with lighters, matches, or fireworks. One way to teach preschool-aged children about objects that might be hot is to create a sorting game where children sort images of items that might be hot or are not hot.
- Keep a fire extinguisher at home, and make sure it’s in working order. Ensure everyone in the family knows where it is, and that those who are old enough know how to use it.
BASIC FIRST AID FOR BURNS:
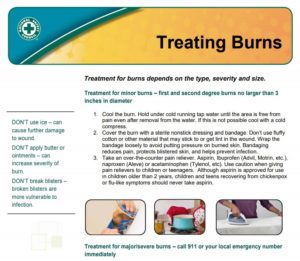
If someone in your family does sustain a burn, it is important to know how to treat it.
- Make sure the person is out of harm’s way and everyone is safe from the cause of the burn.
- Remove any clothing, jewelry, belts, or other items that are near or possibly restricting the burned area. Do this quickly, before the burn swells.
- For minor burns (under 3 inches), run the burn under cool (not cold!) water to help cool the area, or apply a cool, wet compress. Do not immerse a large burn in water.
- For major burns (burns that are deep, have caused a dry and leathery area on skin, or are charred, or burns larger than 3 inches), seek immediate medical care.
- Bandage or cover the burn with a loose, clean cloth to protect the area and keep air off it. Make sure the bandage is not putting pressure on the burn.
- Provide an age-appropriate dose of a pain reducer, as needed, in order to help with the pain of the burn.