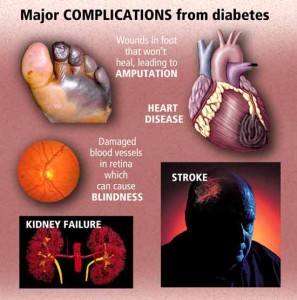
The economic impact of diabetes remains a tremendous burden in the United States. The total economic encumbrance is more than $174 billion annually. The majority of the expenses, $116 billion, were for direct medical costs such as hospital care, emergency room visits, physician office visits and home health visits. The other $58 billion was attributed toward indirect costs such as disability, loss of workplace productivity and premature mortality. According to recent data published by the National Institute of Diabetes and Digestive and Kidney Diseases, most of the expenses associated with diabetes are for long-term complications, such as heart failure, renal failure, hypertension, amputation and blindness. In fact, medical expenses for people with diabetes are twice as high than for people without diabetes. Why not prevent getting it before you here by your doctor your with the diagnosis diabetes. Then you won’t be paying medical expenses twice as high like those who do with diabetes plus you’ll be helping the American economy with decreasing billions put out to expenses of diabetes.
Race and ethnicity also play a role as potential risk factors for diabetes. The most recent National Institutes of Health (NIH) surveys revealed Hispanic Americans and African Americans have a greater prevalence of diabetes than Caucasians (11.8% and 12.6% versus 7.1%). Asian Americans with diabetes make up about 8.4% of all diagnosed cases. Diabetes prevalence in American Indians and Alaska Native in the United States is over twice as high compared to Caucasians (16.1%).
Types of diabetes:
Type 1 diabetes
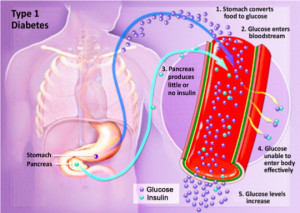
Historically, type 1 diabetes (T1DM) was labeled as insulin dependent diabetes or juvenile diabetes. The WHO and the American Diabetes Association changed the nomenclature due to the evolution of treatment options. The classification is now based on pathogenesis instead of the requirement of insulin therapy. Over 95% of people with T1DM develop the disease before the age of 25.
Type 1 Diabetes is considered an autoimmune disorder and occurs when the pancreas fails to produce insulin. During T1DM, the pancreatic beta cells are damaged or destroyed, which causes insulin to decline. This lack of insulin causes blood glucose levels to rise. During this state, known as hyperglycemia, glucose levels are elevated in the blood and the unutilized sugar is excreted in the urine. This accumulation of glucose in the bloodstream prevents it from going into the cells. This results in the body’s inability to convert the glucose into energy and eventually leads to the symptoms of T1DM.
Risk Factors for Type 1 Diabetes
The risk for developing T1DM can be calculated by measuring molecules, known as biomarkers, which reveal potential autoimmune reactions in the pancreas. Although the exact cause of the autoimmune response in T1DM is unknown, evidence suggests several risk factors, which may enhance the susceptibility for the disease.
Genetic Factors
Researchers have located certain genetic chromosomes and genes, which are related to T1DM. The majority of these genes are referred to as human leukocyte antigen (HLA) genes, they also are responsible for approximately half the genetic risk for T1DM.
Environmental Factors
Research published by the National Center for Biotechnology Information, U.S. National Library of Medicine revealed that the environment plays a role on the development and progression of T1DM.
Certain viruses have been linked to the onset of T1DM. Mumps, rubella and herpes viruses appear to increase the chance of autoimmunity, which precipitates T1DM in people with predisposed autoimmunity. How to prevent this is through rubella and mumps vaccines. There is a relationship between human enterovirus (HEV) infections and the induction of beta cell autoimmunity, which is strongly linked to T1DM. HEVs are small virus particles with more than 100 known different strains
One interesting study by Roivainen and Klingel investigated the link between day care exposure and the incidence of T1DM. Although communal places such as day care facilities, preschool and playgrounds strikes fear in many “germaphobe” parents, several well-designed case control studies have indicated that early social mixing, as in the case at day care, offers protective mechanisms against childhood diabetes. Researchers in these studies believe that exposure to infections in infancy help to strengthen immunoregulatory functions that have a protective effect against diabetes in children before the age of five. Another environmental factor concerning T1DM has to do with the so-called “hygiene hypothesis,” which proposes that T1DM incidence in most industrialized societies is less due to the reduced risk of parasites.
Type 2 diabetes mellitus (T2DM) occurs most frequently in adults over 40 years of age. Prior to being changed by the WHO, T2DM was previously known as adult-onset diabetes, insulin-insensitive diabetes and non-insulin dependant diabetes. In recent years there has been a dramatic increase in the incidence of T2DM. Recent statistics published by the CDC reported that over 285 million people currently have T2DM in the United States. In fact, T2DM is the most common non-communicable disease in the world.
T2DM is characterized by elevated levels of glucose in the blood. Insulin resistance is the primary contributor toward T2DM.
Insulin resistance is the primary contributor toward T2DM. During T1DM, the islet cells in the pancreas are destroyed resulting in the depletion of insulin. Conversely, during T2DM there may be a normal amount of circulating insulin in the body, however, the body’s muscles, fat and liver become resistant or do not use insulin effectively. This condition is called insulin resistance. Insulin resistance can begin in the components of the intercellular cascade, which connects the insulin receptors in the cell membranes. Unlike in the case with T1DM, at least initially, people with T2DM typically do not need insulin to survive.
In normal glucose regulation, insulin stimulates peripheral glucose uptake through the muscles and fat. At the same time, it inhibits glucose production in the liver. During this process, the gastrointestinal (GI) tract helps to transport the glucose into the body during digestion. Conversely, in an environment of impaired glucose tolerance, GI absorption of glucose aggravates already compromised glucose regulatory systems and overpowers the body’s other organs. Because the organs are overwhelmed, they are unable to excrete the surplus glucose, which results in hyperglycemia. T2DM also frequently causes hyperinsulinemia, which is characterized by excess insulin in the bloodstream. Also, during T2DM, the liver both overproduces and underuses glucose. Hyperglycemia causes injury to the beta cells in the pancreas, which makes it even more difficult for the pancreas to regulate the elevated levels of blood glucose. Over time, this process causes harm to blood vessels, nerves, eyes, kidneys and other organs of the body.
T2DM is a heterogeneous disease and can be attributed to a variety of causes. For example, many patients with T2DM are obese, and obesity alone often causes insulin resistance. The potential for developing T2DM increases certain genetic influences and environmental factors such as obesity, dietary factors, age, sedentary lifestyle, smoking and excessive alcohol consumption.
Genetic Factors
According to the National Diabetes Clearinghouse, genetics play a significant role in people with diabetes. Having certain inheritable genes can definitely increase susceptibility to T2DM. Current research has identified over 36 genes that have been associated with the development of T2DM. These genes influence insulin production rather than insulin resistance. One gene identified through research is known as the TCF7L2 gene. People with this gene have an 80% increased risk of developing T2DM compared to those who do not carry the gene. In fact, TCF7L2 is considered the most dominate gene related to the vulnerability of T2DM. Twin studies have also shown that if one identical twin has diabetes, the likelihood of the other twin contracting the disease is approximately 90%. One landmark study of identical twins revealed a 100% concordance rate for the disease.
The pathogenesis of genetic susceptibility is typically related to genetic irregularities related to glucose metabolism. Candidate genes involved in insulin secretion of beta cells play a role in these genetic abnormalities. Researchers have also linked genetic risk to mitochondrial genes and insulin receptor genes. One recent genome-wide association study by Morgan (2012) has recognized the mutation in the KCNQ1 gene, which is related to insulin secretion. The results of this study concluded that this specific gene played a significant role as a genetic risk factor for T2DM in Asian ethnic groups, who were the participants in the investigation.
Obesity
Obesity is one of the strongest risk factors related to insulin resistance and T2DM. According to research reported in The Journal of Clinical Endocrinology & Metabolism, obesity is present in the majority of patients with T2DM. In fact, obesity accounts for almost 85% of the overall risk of developing T2DM. In fact, obesity accounts for almost 85% of the overall risk of developing T2DM. Obesity can be attributed toward eating and lifestyle habits, genetics, or a combination of all three factors. However, one thing is certain – obesity is a major dilemma in the United States and it is been cited as one of the leading major health issues over the past couple decades. According to the U.S. CDC, over one third (35.7%) of adults in America are obese.
The statistics are frightening. According to recent government reports, childhood obesity has tripled over the past 30 years, partly due to the lack of activity. Less than 25% of high school students are engaged in the proper amount of moderate-intensity physical activity.
An abundance of visceral fat is directly associated with insulin resistance. This type of fat is characterized by intra-abdominal fat or “belly fat,” rather than subcutaneous fat or gynecoid “pear shaped” fat, which usually manifests in the thighs and gluteal regions of the body. The intraperitoneal fat drains to the liver and leads to excessive free fatty acid in the bloodstream. This process is one of the causes of insulin resistance.