
What is Epilepsy with a etiology; a neurological disorder with a metabolic or systemic cause. As long as it is controlled like most other diseases you can live a normal life like anyone else. A seizure is a physical manifestation of paroxysmal and abnormal electrical firing of neurons in the brain. Think of it as numerous voltage (hyperexcitability of neurons) going throughout the brain meaning brain waves going in all directions with the brain saying its too much activity. In simpler terms the brain is saying I don’t know what to do, too much brain wave excitability for the organ to register in what to do and freaks out causing the brain to go into a seizure.
Most people with epilepsy are otherwise healthy; as long seizure occurs there is a decrease in oxygen since the brain isn’t capable to send messages during the seizure. If the seizure continues to repeat one right after another the person is in status epilepticus and if the seizures do not stop the person can lead to a neuronal death; like John Travolta’s son who died of this for example.
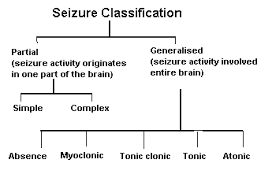
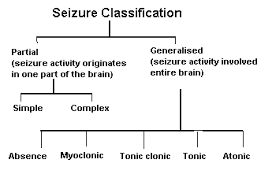
The term seizure disorder may refer to any number of conditions that result in such a paroxysmal electrical discharge. These conditions could be metabolic or structural in nature.
For example, if the cause is metabolic this could be “Canavan disease” which is primarily a disease of demyelination. Your myelin sheath that protects and insulates the nerves is being destroyed and can cause a seizure as one of the symptoms.
*Another example of epilepsy being caused by a metabolic reason is thought to be caused by brain acetate deficiency resulting from a defect of N–acetylaspartic acid (NAA) catabolism (meaning breakdown is occurring). Accumulation of NAA, a compound thought to be responsible for maintaining cerebral fluid balance, can lead to cerebral edema and neurological injury, like a seizure as one symptoms of the disease.
*A structural condition to cause a seizure could be a tumor in the brain. Than there is just idiopathic, unknown cause for the epilepsy which if starts in childhood can resolve by the child growing out it, like in petite mal seizures but it not it goes into motor/focal or grand mal that is permanent the individual needs Rx for life.
Remember, etiology (the cause) of Epilepsy can be generally a sign of underlying pathology involving the brain–knowing the cause. To find this out diagnostic tooling be a neurologist who specializes in epilepsy is the best resource to go to. The epilepsy may be the first sign of a nervous system disease (ex. Brain tumor), or it may be a sign of a systemic or metabolic derangement. Where the treatment may be able to resolve the seizure symptom completely where this wasn’t a seizure disorder or epilepsy but just a symptom due to another disorder that may be 100% cured, like a operable tumor removed surgically from the brain.
Metabolic and Systemic Causes of Seizures:
a.) Electrolyte Imbalance=In the blood having acidosis, heavy metal poisoning, Hypocalcemia (low Ca+) , Hypocapnea (low carbon dioxide), Hypoglycemia (low glucose), Hypoxia (low oxygen), Sodium-Potassium imbalance, and than Systemic diseases (liver, renal failure, etc…). Then their is also toxemia of pregnancy, and water intoxication.
b.) Infections like meningitis, encephalitis, brain abcess.
c.) Withdrawal of sedative-hypnotic drugs=Alcohol, Antiepileptic drugs, Barbiturates, Benzodiazepines.
d.) Iatrogenic drug overdose=Theopylline, Penicillin.
Other causes of epilepsy can be Trauma, Heredity.
Structural causes of epilepsy:
Head trauma/Degenerative Disease like Alzheimer’s or Creutfeldz-Jacob or Huntington’s Chorea or Multiple Sclerosis or Pick’s Disease. There is also tumors or genetic disease or Stroke or Infections or Febrile seizures.
Come back tomorrow for Epilepsy going further on etiology factors for the disease of occur.