What is Endometriosis?
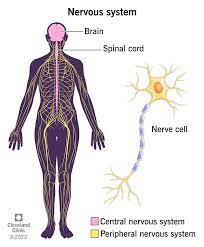
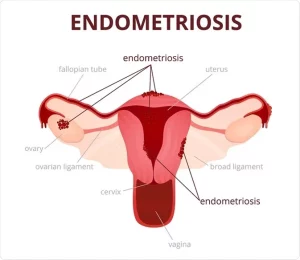
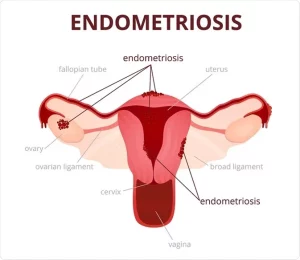
The uterus is a female reproductive organ located between the bladder and the rectum, in the pelvic area. The uterus has three layers: the inner lining (endometrium); the middle muscular layer (myometrium); and the outer layer (perimetrium). The uterus is connected to the fallopian tubes, the cervix and (via the cervix) the vagina.
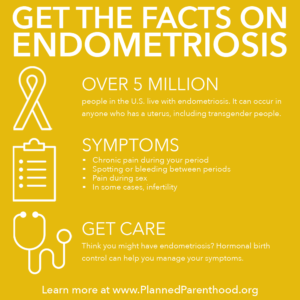
Endometriosis is a painful, chronic disease that affects at least 6.3 million women and girls in the U.S., 1 million in Canada, and millions more worldwide. It occurs when tissue like that which lines the uterus (tissue called the endometrium) is found outside the uterus. The symptoms occur during menses and the endometrial tissue outside the uterus will be painful like the uterus cramps due to the period.
What Causes Endometriosis?
The cause of endometriosis is unknown. The retrograde menstruation theory (transtubal migration theory) suggests that during menstruation some of the menstrual tissue backs up through the fallopian tubes, implants in the abdomen, and grows. Some experts believe that all women experience some menstrual tissue backup and that an immune system problem or a hormonal problem allows this tissue to grow in the women who develop endometriosis.
Another theory suggests that endometrial tissue is distributed from the uterus to other parts of the body through the lymph system or through the blood system. A genetic theory suggests that it may be carried in the genes in certain families or that some families may have predisposing factors to endometriosis.
Surgical transplantation has also been cited in many cases where endometriosis is found in abdominal scars, although it has also been found in such scars when accidental implantation seems unlikely.
Another theory suggests that remnants of tissue from when the woman was an embryo may later develop into endometriosis, or that some adult tissues retain the ability they had in the embryo stage to transform reproductive tissue in certain circumstances.
Research by the Endometriosis Association revealed a startling link between dioxin (TCCD) exposure and the development of endometriosis. Dioxin is a toxic chemical byproduct of pesticide manufacturing, bleached pulp and paper products, and medical and municipal waste incineration. The EA discovered a colony of rhesus monkeys that had developed endometriosis after exposure to dioxin. 79% of the monkeys exposed to dioxin developed endometriosis, and, in addition, the more dioxin exposure, the more severe the endometriosis.
Endometriosis tissus found outside of the uterus:
- Outside and back of your uterus.
- Fallopian tubes.
- Ovaries.
- Vagina.
- Peritoneum (the lining of your abdomen and pelvis).
- Bladder and ureters.
- Intestines.
- Rectum.
- Diaphragm (a muscle near the bottom of your chest that plays an important role in breathing).
- Less commonly they are found in the lung, arm, thigh, and other locations.
This misplaced tissue develops into growths or lesions which respond to the menstrual cycle in the same way that the tissue of the uterine lining does: each month the tissue builds up, breaks down, and sheds. Menstrual blood flows from the uterus and out of the body through the vagina, but the blood and tissue shed from endometrial growths has no way of leaving the body. This results in internal bleeding, breakdown of the blood and tissue from the lesions, and inflammation — and can cause pain, infertility, scar tissue formation, adhesions, and bowel problems.
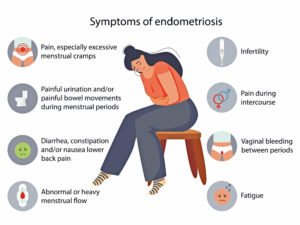
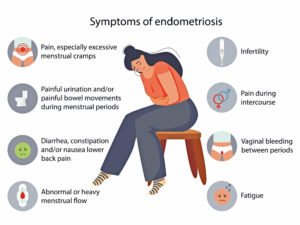
Pain before and during period: Pain with sex, Infertility, Fatigue, Painful urination during periods, Painful bowel movements during periods and Other Gastrointestinal upsets such as diarrhea, constipation, nausea.
In addition, many women with endometriosis suffer from:
- Allergies
- Chemical sensitivities
- Frequent yeast infections
Diagnosis:
Diagnosis is considered uncertain until proven by laparoscopy, a minor surgical procedure done under anesthesia. A laparoscopy usually shows the location, size, and extent of the growths. This helps the doctor and patient make better treatment choices.