“GOUT DIET GOALS:
Achieve a healthy weight and good eating habits
Avoid some, but not all, foods with purines
Include some foods that can control uric acid level
A good rule of thumb is to eat moderate portions of healthy foods.
DIET DETAILS:
uric acid levels and reduce the number of gout attacks is your goal!
The general gout-diet recommendations:
- Weight loss. Being overweight increases the risk of developing gout, and losing weight lowers the risk of gout. Research suggests that reducing the number of calories and losing weight — even without a purine-restricted diet — lower the uric levels and lessens the overall stress on joints.
- Complex carbs. Eat more fruits, vegetables and whole grains, which provide complex carbohydrates. Avoid foods and beverages with high-fructose corn syrup, and limit consumption of naturally sweet fruit juices.
- Water. Stay well-hydrated by drinking water.
- Fats. Cut back on saturated fats from red meat, fatty poultry and high-fat dairy products.
- Proteins. Focus on lean meat and poultry, low-fat dairy and lentils as sources of protein.
- Organ and glandular meats. Avoid meats such as liver, kidney and sweetbreads, which have high purine levels and contribute to high blood levels of uric acid.
- Red meat. Limit serving sizes of beef, lamb and pork.
- Seafood. Some types of seafood — such as anchovies, shellfish, sardines and tuna — are higher in purines than are other types. But the overall health benefits of eating fish may outweigh the risks for people with gout. Moderate portions of fish can be part of a gout diet.
- High-purine vegetables. Studies have shown that vegetables high in purines, such as asparagus and spinach, don’t increase the risk of gout or recurring gout attacks.
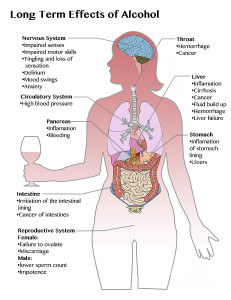
- Alcohol. Beer and distilled liquors are associated with an increased risk of gout and recurring attacks. Moderate consumption of wine doesn’t appear to increase the risk of gout attacks. Avoid alcohol during gout attacks, and limit alcohol, especially beer, between attacks.
- Sugary foods and beverages. Limit or avoid sugar-sweetened foods such as sweetened cereals, bakery goods and candies. Limit consumption of naturally sweet fruit juices.”
MAYO CLINIC (https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524)