
Life can be stressful—you may feel stressed about performance at school, traumatic events (such as a pandemic, a natural disaster, or an act of violence), or a life change. Everyone feels stress from time to time.
What is stress?
Stress is the physical or mental response to an external cause, such as having a lot of homework or having an illness. A stressor may be a one-time or short-term occurrence, or it can happen repeatedly over a long time.
What is anxiety? Anxiety is your body’s reaction to stress and can occur even if there is no current threat.
Trigger Reactions to Stress by the human body:
Increased heart rate and respirations. Increased blood pressure. Upset stomach, nausea, diarrhea. Increased or decreased appetite which may be accompanied by weight loss or gain.
If that anxiety doesn’t go away and begins to interfere with your life, it could affect your health. You could experience problems with sleeping, or with your immune, digestive, cardiovascular, and reproductive systems. You also may be at higher risk for developing a mental illness such as an anxiety disorder or depression.
Everyone experiences stress, and sometimes that stress can feel overwhelming! You may be at risk for an anxiety disorder if it feels like you can’t manage the stress and if the symptoms of your stress:
- Interfere with your everyday life.
- Cause you to avoid doing things.
- Seem to be always present.
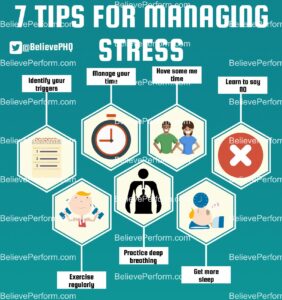
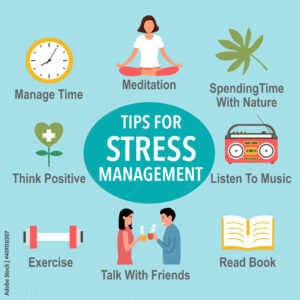
Learning what causes or triggers your stress and what coping techniques work for you can help reduce your anxiety and improve your daily life. It may take trial and error to discover what works best for you. Here are some activities you can try when you start to feel overwhelmed.
What to do if stress triggers and to help yourself ; when picking up on it; some ideas:
- Keep a journal.
- Download an app that provides relaxation exercises (such as deep breathing or visualization) or tips for practicing mindfulness, which is a psychological process of actively paying attention to the present moment.
- Exercise, and make sure you are eating healthy, regular meals.
- Stick to a sleep routine, and make sure you are getting enough sleep.
- Avoid drinking excess caffeine such as soft drinks or coffee.
- Identify and challenge your negative and unhelpful thoughts.
- Reach out to your friends or family members who help you cope in a positive way.
One way of looking at life is whatever challenges comes your way know you will survive and for any losses you may experience when looking back on them take the positive aspects or memories not the negative that builds a bad effect on you (Ex. Insomnia to depression to high blood pressure to alcoholism to drugs).
A positive effect can be as simple as a smile when reflecting memories, which FYI allows less frowning that will cause less wrinkles on the forehead, as we get older. Sometimes it’s not that simply and when it gets harder take up a constructive way of dealing with it (Ex. Work out at your level, walking, singing, go to a comedy movie, get together with friends go out, and do anything that gets your mind off of the stress and even out of your body through work out at the gym to just biking or walking.).
For starters stress is a body reaction to CHANGE. How to you look at change? Easy, positive in someway! It may not appear easy at first but try to look at this change as a sense of difficulty yet a challenge with a victory in the end, if approached right.
Let us take the following challenges we face in life, for example – Having a child leave home for college or marriage, losing a home with this economy, a loss of a friend in your life: How do you look at these experiences positive?
1.) Well for the child I would be so happy for her or him starting college life with my worries but know I raised her or him well and if he makes mistakes on the way he or she will learn to get up off the ground and fix them knowing he or she can come to me or dad whenever he has the need or if we sense a problem we would address it (Its part of life=growing up).
2.) Another aspect to look at regarding this stress is there is loss in the parent role so fill up that loss with a new hobby, or get active in whatever organization you are in (Ex. Church, Temple, School, to just taking up ceramics or do more traveling with your spouse and friends). Help out the community you live in and assist in organizations that you feel do help the society in your city or town or village you live in. I had my falls with the stresses that I have come across in my lifetime but you got to get up every time to stand again, some quicker than other times. Love ones we loose I deal with in a positive way in knowing their in heaven, a lot better than here also looking at the fond memories I have of that person with knowing I will see them again when I pass on but trying to keep active with my life which now is hard but with my significant other helping me to get started.
3.) How do you deal with losing a home with this economy or a business as well appreciate the good memories you had when you had the home and pick up starting a new life elsewhere with making it a journey down the yellow brick road leading you to where the rainbow is at the end; don’t look at it as a loss. It may be miserable at first but being a nurse seasoned I know there is always someone worse than I am and no I am not rich (far from it) that I can pick up and by another home.
4.) If you lost a business in the time of COVID-19 due to this long stretch of lockout particularly in NY (take the city alone) or if you just lost a business in general. It is a hard challenge to come across but there is a new plan and journey for you to restart. My family was there in losing business or a job including my husband in this COVID-19 but we resolved all job problems and with saving our money, it took time, but we survived. We have each other and thank God we never lost our home we can say. We can make through anything as long as we have each other and this is not a happy episode of “Little house on the Prairie” but knowing how to look at life’s challenges positive with negative feelings at first, which is only expected.
The same as Erickson’s stages of death; first denial to anger to bargaining to depression to acceptance and will relive these steps over again during your challenge but will beat it with having a positive approach and knowing how to use effective methods to let your stress go. Know you will have those Erickson steps replaying over, not even in those steps directly 1 through 5 but know what to do when you relive them like work out, go to a volunteer organization and help out or whatever makes you feel better that does not hurt your health but help it in a positive approach.
Dealing with losing a friend or terminal friend, again the way I look at it is I appreciate the time I had with her or him and know they haven’t left me in spirit (if deceased). If the person is still living know there are reasons for everything; whatever the cause was for the reason for the relationship in parting, divorce or death for example. When out of my control I think of how I had a good friendship as opposed to never having one with that individual or thinking I will never see them again. I accept that nothing lasts forever or indefinitely, with appreciating the time I had with the person and money is just monetary with hoping it gives me good memories if I loose or choose to ever leave it (like a home, car, etc). I try to cherish each day for being given that gift by God to have ever have met that person and was able to spend time with that person.
Ending note, I look at life this way, whatever positive entity comes in my life may be taken away from me and I should appreciate every moment I spend with that person or creature or career or job or home in my life that I love so much (including my life span that only upstairs knows how long that time factor will be but I try to live a life at its healthiest optimal level with practicing positive behavior which is knowing whatever stressors come my way there is always someone is worse off and thank God for the life I was given which makes me a strong person in facing everything that has come my way, so far. What has probably helped me is being a RN for over 35 years and working in so many specialty areas that made me see people worse off than me in health and more.
If I don’t deal with stress like this than I can expect complications that may arise, just like for anyone else who looks at challenges coming their way in a negative sense. You commonly see stress become a negative experience when a person faces continuous challenges/stressors without relief or relaxation between them. The ending result is the person becomes overworked and stress-related tension builds. Stress that continues without positive resolution at some level can cause a condition called distress, which is a negative stress reaction.
The physical reactions that happen to your body due to negative stress can be = negative symptoms there is both acute vs chronic.
Stress is a normal part of life; the ones you build up one over another with no resolving them make the stress worse!
Acute VS Chronic Stress to the human body:
Many events that happen to you and around you — and many things that you do yourself (Ex. Work 40 to 60 hrs a week in a highly stressful job, like a policeman) – will put stress on your body.
You can experience stress from your environment, your body, and your thoughts. You can also cause the stress to impact your body with first just signs and symptoms (s/s) developing, that are listed above, but without relief of the stress these s/s can lead you into a disease/illness forming or even make the diagnose (s) you already have even worse.
Many signs and symptoms pick up when exposed to continual stress or stresses that just build up on top of each other causing some people in developing unhealthy habits, poor dieting, and the lack of desire to be as active as they were which in turn develops conditions that would not have occurred if this negative behavior didn’t happen over a long period of time which has occurred to me and come back but get on top of it or it gets harder to beat!!
This behavior with the stress or stresses you are experiencing increases the probability of health conditions starting to take place in your body or if you’re with certain diagnoses already the stress can possibly impact your body by worsening the condition.
1.) Acute Stress to the human body ( a stress response over short term, immediately reacting):
-Elevated high blood pressure –Headaches –Chest Pain –Upset Stomach –Insomnia –Grinding of the teeth –Jaw Tension –Teeth grinded down –Irritability –Anger –Panic episodes –Vasoconstriction to our vessels causing increases to the heart rate –Decreases sex drive –Depression (Research even suggests that stress also can bring on or worsen certain symptoms or diseases.)
Stress costs American industry more than $300 billion annually. The lifetime prevalence of an emotional disorder is more than 50%, often due to chronic, untreated stress reactions.
2.) Chronic Stress to the human body (a stress response over long term stress=medical conditions arrising):
-ADD or ADHD –Panic disorders –High blood pressure –Anti-arrhythmias -Cardiac Disease -Diabetes 1 or Diabetes 2 -Stroke –Irritable Bowel Syndrome –Weight Gain/Obesity –Fibromyalgia –Complex Regional Pain Syndrome –ETOH -Depression and so much more.
Learn how to beat stress and help your health and no one can do it but do! Today we learned what stress is, trigger reactions by the body in stress, what to do if it triggers, the symptoms immediate vs. long term stress challenges we come across in life. Check out tomorrow’s topic Part II – tips on dealing with stress!
.