
In 2013, America’s 55 poison centers received over 3.1 million calls. Of those, about 2.2 million were calls about poison exposures ranging from carbon monoxide to snake bites to food poisoning. The rest were calls for information.
Chemicals in and around the home can poison people or pets and can cause long-term health effects. Every 13 seconds, a poison control center in the United States answers a call about a possible poisoning. More than 90% of these exposures occur in the home. Poisoning can result from medicines, pesticides, household cleaning products, carbon monoxide, and lead.
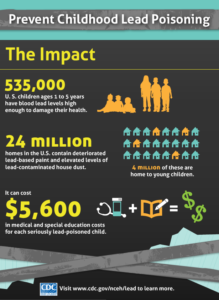
The major source of lead poisoning among U.S. children is lead-based paint and dust with lead. All houses built before 1978 are likely to contain some lead in the paint. However, it is the flaking, peeling paint that causes a problem. Other sources of lead in the home may include traditional home remedies, ceramics, toys and toy jewelry, lead-contaminated soil, lead water pipes, and lead solder used in plumbing. Lead poisoning occurs when lead builds up in the body, often over a period of months or years. Even small amounts of lead can cause serious health problems. Children under the age of 6 are especially vulnerable to lead poisoning, which can severely affect mental and physical development. At very high levels, lead poisoning can be fatal. While treatment is available for lead poisoning, taking some simple precautions can help protect yourself and your family.
Lead-based paint and lead-contaminated dust in older buildings are the most common sources of lead poisoning in children. Other sources include contaminated air, water and soil. Adults who work with batteries, do home renovations or work in auto repair shops also may be exposed to lead. It couldn’t hurt to ask you MD if you should get a lead level taken yearly or less for people who live around lead or the area having a history of it or adults in the work force working need lead products.
Lead poisoning symptoms in children
The signs and symptoms of lead poisoning in children may include:
Developmental delay-Learning difficulties-Irritability-Loss of appetite-Weight loss-Sluggishness and fatigue-Abdominal pain-Vomiting-Constipation-Hearing loss
Lead poisoning symptoms in newborns
Babies who are exposed to lead before birth may experience:
Learning difficulties & Slowed growth
Lead poisoning symptoms in adults
Although children are primarily at risk, lead poisoning is also dangerous for adults. Signs and symptoms in adults may include:
High blood pressure-Abdominal pain-Constipation-Joint pains-Muscle pain-Declines in mental functioning-Pain, numbness or tingling of the extremities -Headache-Memory loss-Mood disorders-Reduced sperm count, abnormal sperm-Miscarriage or premature birth in pregnant women.
ENDING LINE is knowing how to prevent leading causes of child injury, like poisoning, helps keep our children safe and secure and helps them live to their full potential.
We all want to keep our children safe and secure and help them live to their full potential. Knowing how to prevent leading causes of child injury, like poisoning, is a step toward this goal.
Every day, over 300 children in the United States ages 0 to 19 are treated in an emergency department, and two children die, as a result of being poisoned. It’s not just chemicals in your home marked with clear warning labels that can be dangerous to children.
Everyday items in your home, such as household cleaners and medicines, can be poisonous to children as well. Active, curious children will often investigate—and sometimes try to eat or drink—anything that they can get into.
Thankfully, there are ways you can help poison-proof your home and protect the children you love.
Prevention Tips
Lock them up. Keep medicines and toxic products, such cleaning solutions, in their original packaging where children can’t see or get them.
Know the number. Put the nationwide poison control center phone number, 1-800-222-1222, on or near every telephone in your home and program it into your cell phone. Call the poison control center if you think a child has been poisoned but they are awake and alert; they can be reached 24 hours a day, seven days a week. Call 911 if you have a poison emergency and your child has collapsed or is not breathing.
Read the label. Follow label directions and read all warnings when giving medicines to children.
Don’t keep it if you don’t need it. Safely dispose of unused, unneeded, or expired prescription drugs and over the counter drugs, vitamins, and supplements. To dispose of medicines, mix them with coffee grounds or kitty litter and throw them away. You can also turn them in at a local take-back program or during National Drug Take-Back events.
In general, Health and Safety Tips
Make sure your child does not have access to peeling paint or chewable surfaces painted with lead-based paint.
Use and store chemicals, household cleaning products, and pesticides according to label instructions and out of reach of children
Have gas appliances professionally installed, vented outside, and checked annually for carbon monoxide leaks.
Take all medicines as directed and store out of reach of children.
Turn on fans and open windows to help ventilate the area when using household cleaners and chemicals.
Deaths from drug overdose have been rising steadily over the past two decades and have become the leading cause of injury death in the United States.
The United States is in the midst of an opioid overdose killed more than 28,000 people in 2014, more than any year on record. At least half of all opioid overdose deaths involve a prescription opioid. More people died from drug overdoses in 2014 than in any year on record. The majority of drug overdose deaths (more than six out of ten) involved an opioid. Opioids include opiates, an older term that refers to such drugs derived from opium, including morphine itself. Other opioids are semi-synthetic and synthetic drugs such as hydrocodone, oxycodone and fentanyl; antagonist drugs such as naloxone and endogenous peptides such as the endorphins. Opioid drugs are predominantly central nervous system agents, most often used medically to relieve pain. So again its restated to take meds as prescribed and keep out of reach for children especially (babies/children out of reach to locked up-Better safe than sorry).